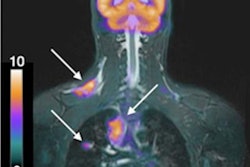
Although FDG-PET/MRI shows promise for accurate staging of breast cancer, the modality still isn't as accurate as sentinel lymph node biopsy, according to a study presented last week at RSNA 2019 in Chicago.
German researchers compared the hybrid modality against breast and whole-body MRI and ultrasound and found that FDG-PET/MRI performed better than the others but could not find lymph node (N) metastases in as many patients as the invasive biopsy procedure.
"We found that FDG-PET/MRI performed best in defining the N status and also has the highest accuracy, compared to the other imaging modalities," added presenter Dr. Lino Sawicki, from the department of diagnostic and interventional radiology at the University of Düsseldorf, Germany. "However, imaging modalities do not reliably differentiate the N-positive and N-negative breast cancers, compared with the gold standard of sentinel lymph node biopsy."
Breast cancer is the most common form of the disease among women worldwide. It accounts for approximately 12% of new cancer diagnoses every year and approximately 27% of women with cancer have the disease in their breasts. It is considered to be one of the leading causes of cancer-related deaths among women. Lymph node metastases are often present, and sentinel lymph node biopsy is regarded as the gold standard to differentiate N-positive or N-negative status.
"The question that we had was whether we can use ultrasound, MRI, or FDG-PET/MRI to directly identify the stage of breast cancer," Sawicki explained to the RSNA attendees. "Can we replace sentinel lymph node resection in breast cancer patients through breast MRI, axillary whole-body MRI, FDG-PET/MRI, or axillary sonography?"
To help answer that question, the researchers performed a two-center prospective study in which they enrolled 56 women (mean age, 53.5 ± 12.2) with newly diagnosed, histopathologically proven breast cancer. The subjects ranged from having T2 cancer, which means the tumor is between 20 mm and 50 mm in size, to having T1c cancer and a molecular high-risk profile.
All patients underwent a dedicated breast MRI scan, FDG-PET/MRI exam, and axillary sonography. Breast and whole-body MRI sequences included T1-weighted dynamic contrast imaging, T2-weighted turbo spin echo, and diffusion-weighted MR imaging (DWI). The FDG-PET/MRI protocol consisted of a postcontrast T1-weighted volumetric interpolated breath-hold exam, T2-weighted half-Fourier acquisition single-shot turbo spin echo, and DWI.
The women's sentinel lymph node biopsy and/or axillary lymph node dissection results served as the reference standard for the imaging modalities. Based on biopsy results, lymph node metastases were present in 25 patients, who had a total of 78 metastases. FDG-PET/MRI found metastases in 19 patients (76%), followed by sonography with metastases in 18 patients (72%), whole-body MRI with metastases in 15 patients (60%), and dedicated breast MRI with metastases in 14 patients (56%).
The researchers' lesion-based analysis determined that axillary FDG-PET/MRI achieved the highest accuracy (78%), followed by sonography (72%), for nodal staging in breast cancer patients.
| Modalities' performances in the detection of 78 metastases | ||||
| FDG-PET/MRI | Breast MRI | Whole-body MRI | Sonography | |
| Sensitivity | 71% | 54% | 55% | 60% |
| Specificity | 92% | 89% | 90% | 86% |
| Positive predictive value | 65% | 89% | 89% | 84% |
| Negative predictive value | 90% | 54% | 53% | 61% |
| Accuracy | 78% | 68% | 57% | 72% |
Sawicki and colleagues concluded that FDG-PET/MRI and sonography achieved "equally acceptable diagnostic accuracy" for nodal staging in breast cancer patients and are "both superior" to dedicated breast MRI and whole-body MRI. Neither FDG-PET/MRI nor sonography, however, could surpass biopsy in finding all 78 metastases in the 25 female patients or "reliably differentiate N-positive from N-negative breast cancer patients," they wrote in their study abstract.
"Therefore, sentinel lymph node biopsy, in our opinion, cannot be replaced by imaging procedures alone and is still needed in the staging for breast cancer patients," Sawicki said.