A whole-body imaging cancer screening program could be an effective way to detect early-stage cancer among a motivated screening population, according to a study from Japan published January 1 in the Journal of the American College of Radiology.
The study implies that although using whole-body imaging to screen for cancer isn't usually top of mind for U.S. clinicians, it may have a place in the cancer prevention arsenal in other parts of the world, wrote a team led by Dr. Yoshimi Anzai of the University of Utah in Salt Lake City.
"Although it may sound unrealistic to offer whole-body cancer screening FDG-PET/CT for asymptomatic healthy subjects, prior reports from Japan and China suggest cancer detection rates between 0.7% and 3.16% for whole-body screening depending on the inclusion criteria and combination of cross-sectional imaging modalities," the group wrote.
Whole-body imaging for cancer screening in asymptomatic patients is challenging in the U.S., due to the high cost of advanced imaging exams, the team noted. But in countries where healthcare is more affordable, it may offer a viable option.
Anzai's group evaluated the effectiveness of a cancer screening program offered at Hamamatsu Photonics, an engineering firm in Hamamatsu, Japan, between 2009 and 2017. The program was prompted by some cancer deaths at the firm in 2002, the authors noted.
"The former ... chief executive officer of the company, Mr. Teruo Hiruma, was seriously concerned when several employees with highly technical skills died from cancer in 2002," the authors wrote. "He envisioned that proactive whole-body cancer screening using advanced imaging technology could lead to longer and healthier lives."
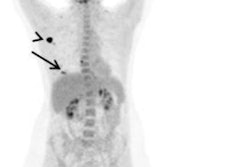
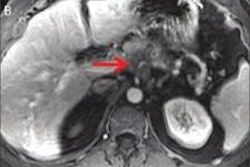
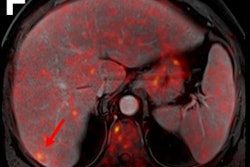
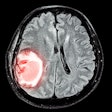
The company started a program that allowed participants to undergo PET/CT, noncontrast brain and pelvis MRI, and abdominal ultrasound exams every two years over a 10-year timespan. Employees could also undergo annual screenings such as chest x-ray, upper gastrointestinal x-ray with oral contrast, fecal occult blood test, prostate-specific antigen testing (for men over 55), and mammography (for women over 40). The program cost $1,350 per employee every two years; this cost was split between the company and participants.
For the imaging exams, employees were categorized into full participation (five screenings), partial (more than once and less than five), and no participation groups. Anzai's team measured the cancer detection rate, rate of cancer-related death, and cancer-related costs of care. Of 1,213 employees, 543 were full participants, 318 were partial, and 352 did not participate in the imaging protocol. Across all three groups, 54 cancers were identified, with the majority in the full and partial participation groups being early stage (0 to 1).
The study showed that whole-body cancer screening did reduce cancer-related mortality and costs of cancer care, but it did not statistically significantly increase the cancer detection rate.
| Cancer detection and cost metrics across three categories of an employee screening program | |||
| Measure | Full participation | Partial participation | No participation |
| Number of cancers identified | 26 | 9 | 19 |
| Cancer detection rate ratio per 100,000 person years | 0.88 | 1.03 | -- |
| Cancer detection per 100,000 person years | 479 | 554.5 | 539.8 |
| Cancer-related mortality per 100,000 person years | 18.4 | 185 | 170.5 |
| Cancer-related mortality rate ratio per 100,000 person years | 0.11 | 1.09 | -- |
| Average cost of cancer care in first year after diagnosis | $19,149 | $26,292 | $45,986 |
| Average total cost of cancer care from diagnosis to October 2019 | $30,901 | $31,998 | $59,953 |
The research suggests that, in the right population, whole-body cancer screening could prove useful.
"Employers with highly skilled employees with very little attrition may be motivated to provide an upfront investment in cancer screening to maintain productivity, reduce loss of employees because of cancer-related deaths and illness, and show their commitment to the overall health of their employees," Anzai and colleagues concluded.