Predicting the success of head and neck cancer treatment, staging it, and addressing its side effects are the focus of three recent papers.
German investigators devised a tumor control model using repeat PET scanning during radiotherapy, while a group from Stanford University offered practical guidelines for performing FDG-PET/CT for this disease. Finally, the North Central Cancer Treatment Group tested the theory that administering zinc sulfate to patients undergoing oral cancer treatment inhibits the loss of taste perception.
Reoxygenation time
For radiotherapy to perform at its peak, rapid reduction of the tumor cell population through reoxygenation is essential, according to Daniela Thorwarth, Ph.D., and colleagues from the University Hospital Tübingen in Tübingen, Germany.
"The presence of regions in a tumor where cells can suffer from a lack of oxygen supply is a symptom of an insufficient or deficient vasculature," the group wrote in the International Journal of Radiation Oncology, Biology, Physics. "If functional imaging reveals the irregularity and coarseness of the tumor vasculature, it may be possible to estimate the time to reoxygenation" (IJROBP, March 28, 2007).
With that in mind, the group developed a model for tumor control based on perfusion efficiency and hypoxia, and measured by PET imaging with F-18 fluoromisonidazole (FMISO-PET).
They enrolled 15 patients with head and neck cancer who underwent FDG-PET and FMISO-PET scans prior to chemoradiation treatment. A subset of 10 patients had repeat scans two weeks into treatment (20 Gy dose for radiotherapy). All patients were treated with 70 Gy delivered in 35 fractions. Post-therapy, all patients were checked every three months with clinical exams and imaging.
According to the results, the authors developed three tumor models:
 |
|
| Tumor type | Characteristics |
 |
|
| Classic hypoxic tumors |
|
| Viable vasculature tumors |
|
| Favorable prognosis tumors |
|
 |
|
The authors drew several conclusions from their results. First, high levels of tracer retention indicate an unfavorable prognosis. Second, the reoxygenation pattern of viable vasculature tumors indicates a faster response to radiotherapy, the authors explained. The rapid response would most likely be caused by a drop in oxygen consumption coupled with acute inflammatory reaction, they added. Finally, the initial degree of hypoxia and reoxygenation speed are linked to vasculature irregularity, with the intervascular spaces defining the areas where hypoxia can happen.
"The speed of reoxygenation ... impacts the strategy of dose escalation that could be adopted to overcome hypoxia-induced radioresistance and the consequential reduction of cell kill," the authors wrote. "Hence, sequential hypoxia images during radiotherapy can be particularly valuable for patients for whom a pretreatment scan predicted slow reoxygenation and consequentially high dose escalation factors."
Thorwarth's group did caution that its model was based on population-averaged reoxygenation dynamics and that individual patients may deviate from these predictions.
PET/CT management
In head and neck squamous cell carcinoma (HNSCC), FDG-PET/CT is a soup-to-nuts modality for initial staging, monitoring therapeutic response, and long-term surveillance, according to Dr. Andrew Quon and colleagues from various departments at Stanford University Medical Center in Stanford, CA. In a review article, Quon and colleagues outlined the role of FDG-PET/CT in HNSCC and also shared their preferred algorithms.
"F-18 FDG-PET/CT can certainly play an important role in identifying disease in lymph nodes in unexpected locations (upper mediastinum and axilla) and detecting unsuspected distant metastatic disease," they wrote (Journal of Nuclear Medicine, January 2007, Vol. 48:1, pp.58S-67S).
For staging HNSCC, Quon's group starts with MRI for detecting the primary tumor, then uses PET/CT for tracking distant metastases. Identifying the primary tumor in HNSCC is vital as it can influence surgical resection or define the extent of radiotherapy. This PET/CT exam can also serve as a baseline scan, even in stage N0 disease, for treatment follow-up.
"PET/CT may be performed before treatment to assess for local-regional disease, distant metastases, or synchronous tumor," they added.
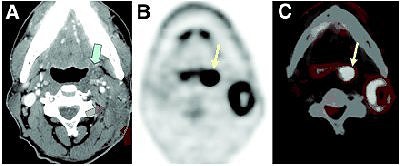 |
| HNSCC metastasis from unknown primary tumor. Patient had enlarging 3-cm left neck mass felt on physical examination. (A) Contrast-enhanced CT depicted space-occupying lesion (green arrows) in left neck. Biopsy of lesion was obtained by fine-needle aspiration, and lesion proved to be lymph node metastatic squamous cell carcinoma. There was no clear evidence of primary tumor except for subtle asymmetry at left tonsillar fossa (blue arrow) that was of uncertain significance. F-18 FDG PET (B) and fusion PET/CT (C) clearly identified primary tumor at left tonsillar fossa (yellow arrows); finding was confirmed by endoscopic biopsy. Quon A, Fischbein NJ, Ross McDougall IR, Le Q, Loo Jr BW, Pinto H, Kaplan MJ, "Clinical Role of 18F-FDG PET/CT in the Management of Squamous Cell Carcinoma of the Head and Neck and Thyroid Carcinoma" (Journal of Nuclear Medicine, Vol. 48, No. 1 (Suppl): 58S-67S). Reprinted by permission of the Society of Nuclear Medicine. |
For monitoring chemoradiation, PET can detect residual tumor post-treatment more accurately than conventional imaging, the group explained. In a 108-patient study conducted at Stanford, PET/CT for locoregional persistent or recurrent HNSCC turned in a sensitivity of 87%, a specificity of 92%, a positive predictive value (PPV) of 64%, a negative predictive value (NPV) of 97%, and an accuracy of 90%. In addition, for detecting distant metastases, PET/CT had a sensitivity of 89%, a specificity of 97%, a PPV of 85%, an NPV of 98%, and accuracy of 96% (Laryngoscope, April 2005, Vol. 115:4, pp. 645-650).
Quon's group suggested that PET/CT be performed two to three months after the completion of radiation therapy to achieve maximum accuracy. They also recommended watching out for nonspecific increase in tracer uptake in the lymphoid tissue, salivary glands, muscles, and soft tissue, generally as a result of post-treatment inflammation.
RT with a zinc chaser
Patients undergoing radiation therapy to the oral cavity often experience a decreased sense of taste and/or a distortion of taste. This in turn can lead to malnutrition, which may affect their ability to recover from their treatment, explained Dr. Michele Halyard, who led the North Central Cancer Treatment Group in a study to determine if the administration of zinc sulfate could prevent therapy-induced taste alterations.
Unfortunately, the results were "disappointing," according to the group.
"Zinc sulfate did not significantly increase the interval to taste alterations, (but) we cannot rule out the possibility that zinc may be exerting some subtle protective effects on taste," wrote Halyard, who is from the Mayo Clinic in Scottsdale, AZ. Her co-authors are from several U.S. institutions, including both Mayo Clinics in Rochester, MN, and Jacksonville, FL (IJROPB, April 2007, Vol. 67:5, pp. 1318-1322).
For this phase III trial, 169 head and neck cancer patients were deemed eligible. They received 2,000 cGy or more of external beam radiation therapy to 30% or more of the oral cavity. Patients were randomly assigned to receive either 45 mg of oral zinc sulfate thrice daily after meals, or a placebo at the same frequency.
Patients were assessed weekly during therapy, then up to six months after treatment completion. The assessment parameters included patient-reported taste alterations (Wickham questionnaire) and physician-reported weight measurements. A 10% decline in taste as reported on the Wickham questionnaire was considered a moderate effect.
Overall, 73% of the zinc-treated patients and 84% of the placebo patients reported taste alterations within the first two months. Their descriptions of how food tasted included "greasy," "soapy," and "powdery." Some also stated that their tongues felt burnt.
This led the authors to conclude that zinc sulfate did not provide any benefit to taste alterations or taste recovery. However, they did note that the median interval to alterations in taste was 2.3 weeks for the zinc group versus 1.6 weeks for the placebo group. While this trial end point did not reach statistical significance, the group noted that zinc has been shown to aid in wound repair and immunity maintenance.
Finally, 99% of the zinc-treated patients maintained their weight, compared with 92% of the placebo patients. While patients did complain of taste alterations, ultimately, this side effect did not affect their reported quality of life, Halyard's group wrote.
Almost a decade ago, Italian investigators at the National Cancer Institute in Milan stated that palliative zinc treatment could become "routine in clinical practice to improve the supportive care of patients with taste alterations resulting from head and neck cancer" (Cancer, May 15, 1998, Vol. 82:10, pp. 1938-1945).
Halyard's group suggested that their current study results may have greater weight because of a larger patient population (169 versus 18), and because their study used the validated Wickham questionnaire.
By Shalmali Pal
AuntMinnie.com staff writer
April 26, 2007
Related Reading
3D radiation can reduce feeding tube need in head and neck cancers, November 9, 2006
IV chemoradiation option for inoperable head and neck cancer, November 9, 2006
Combined approach often effective for head and neck cancer, August 11, 2006
Brain outwits buds in determining what tastes great, March 22, 2006
PET zeros in on hypoxia in head and neck cancer treatment, April 10, 2002
Copyright © 2007 AuntMinnie.com