While MRI is known to detect more myocardial scarring than PET in patients with occlusive coronary artery disease (CAD), a new study suggests that contrast-enhanced MRI can make a critical difference in treatment planning for those revascularization candidates who have severely impaired left ventricular (LV) function.
In their study, Dr. Peter Hunold and colleagues from University Hospital Schleswig-Holstein in Lübeck and the University of Duisburg-Essen in Essen, Germany, found that even though the two modalities performed similarly in most patients, those with the most severe LV dysfunction were more likely to benefit from the use of MRI for revascularization planning.
"These are the patients who really matter because they have a higher rate of risk and lower functionality after revascularization," Hunold said in a presentation at the 2008 RSNA meeting in Chicago.
Viability imaging is important for therapy planning in patients with coronary artery disease, he said. Although late gadolinium enhancement in MRI is an established method of detecting myocardial scarring, FDG-PET, the former reference standard for myocardial scar detection, is still commonly used.
"There is, of course, a negative correlation between the scar extent and functional recovery," he said.
Hunold and his colleagues, including Dr. Alexander Marcin, Dr. Thomas Schlosser, and Dr. Roman Pink, aimed to evaluate late gadolinium enhancement in contrast-enhanced MRI and compare it to FDG-PET for imaging of myocardial viability in CAD, assessing the reliability of the two techniques in patients with different levels of LV function.
They used FDG-PET and contrast-enhanced MRI to scan 105 patients with occlusive coronary artery disease (87 men, 18 women; mean age 61 ± 11 years) who were scheduled for coronary artery bypass graft (CABG) surgery. All patients had a clinical indication for viability PET. A functional contrast-enhanced MRI study was added for comparison purposes with patients divided into three groups with different levels of LV function: ejection fraction (EF) less than 30%, EF 30% to 50%, and EF greater than 50%.
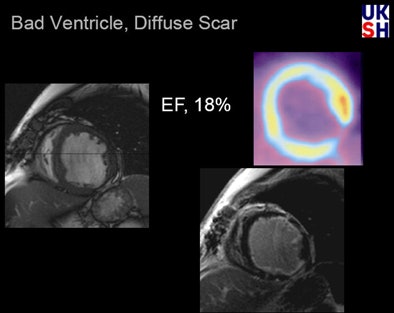 |
| In a patient with severely impaired LV function (EF 18%), PET reveals a small transmural scar at the inferior lateral wall, as well as an apparent FDG uptake deficit. MRI of the same patient shows a small transmural scar and a large subendocardial scar indicating typical ischemic cardiomyopathy. All data and images courtesy of Dr. Peter Hunold. |
MRI imaging at 1.5 tesla (Sonata, Siemens Healthcare, Erlangen, Germany) included a 2D true-FISP functional study of the entire LV eight to 15 minutes following administration of 0.2 mmol/kg body weight of Gd-DTPA (Magnevist, Bayer HealthCare Pharmaceuticals, Wayne, NJ). This was followed by a segmented IR turboFLASH sequence (TR, 8 msec; TE, 4 msec; TI, 200-240 msec) to detect late gadolinium enhancement, which was classified on a four-point scale (1 = normal, 2 = greater than 50% of maximum, 3 = less than 50% of maximum, and 4 = no uptake).
PET was performed on a Siemens ECAT HR+ scanner following administration of 370 MBq [F-18]-FDG with evaluation of reformatted PET 3D datasets.
Results for 105 patients showed that 45, 44, and 16 had ejection fractions less than 30%, 30% to 50%, and greater than 50%, respectively. Of 5,508 segments evaluated, 2,474 (45%) showed late gadolinium enhancement in MRI (score 2/3/4: 915/679/880), Hunold stated. PET showed uptake deficits in 2,220 (40%) patients (score 2/3/4: 1,108/581/531).
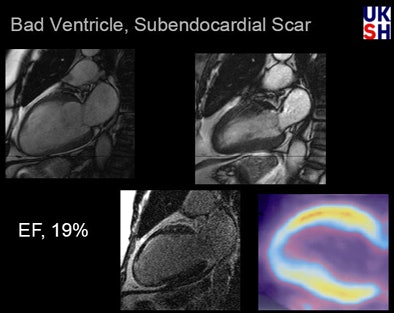 |
| In a patient with three-vessel disease and severely impaired LV function (EF 19%), PET missed a very small scar seen on the anterior wall at MRI. However, the small size of the scar suggests an excellent prognosis. |
MRI predicted better outcomes than PET in patients with normal myocardium or only minor scarring (viability scores 1 and 2), Hunold said. On the other hand, "when it comes to those scars and deficits that are not expected to recover in function [scores 3 and 4], MRI was a little less optimistic than the PET scan," he said.
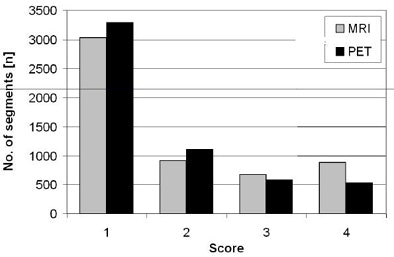 |
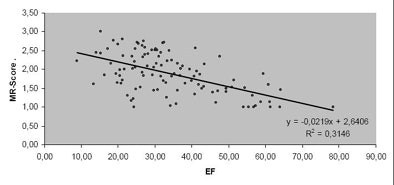
| In myocardial segment viability chart (above), MRI predicted better patient outcomes than PET in patients with normal myocardium or only minor scarring (viability scores 1 and 2). Conversely, in patients with more extensive scarring (viability scores 3 and 4), MRI predicted less functional recovery after revascularization compared to PET. Chart below shows correlation between scar extent at MRI and LV function. |
 |
When scar detection was broken down by percentage of scarred segments in the three patient groups with different levels of LV function, "the group with the least global function [< 30% EF] had a higher percentage of scar detected by MRI than PET," Hunold said. "On the opposite side, in patients with normal or nearly normal LV function there was less scarring detected by MRI."
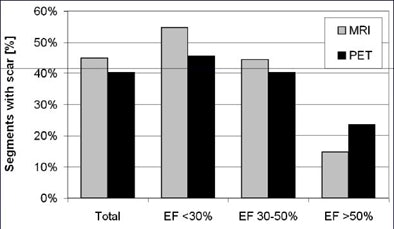 |
| Scar detection chart for patients scored 2, 3, or 4 for myocardial segment viability, respectively, shows that MRI found more myocardial scarring than PET. |
Finally, an analysis of the agreement between the modalities showed that in patients with "normal or nearly normal EF, there is homogeneity in around 70% of cases, and in only a few studies were more scars seen in MRI compared to PET," he said.
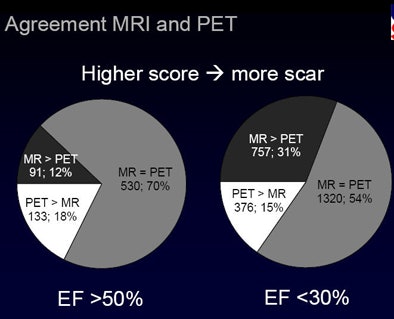 |
| Overall agreement between MRI and PET was relatively high (70%) in patients with normal or near-normal LV function, but fell to 54% in the group of patients with severely impaired LV function (EF < 30%). |
The results bode well for MRI because patients with the most severe dysfunction need the improved scar detection it provides, given their greater overall risk and generally poorer outcomes after revascularization, Hunold said.
"MRI detects more scarring than PET does -- that has been known from the literature for the last couple of years," he said. "But there seems to be significant disagreement [between MRI and PET] in patients with moderately or severely impaired LV function."
PET seems to overestimate functional recovery while MRI is a little bit more cautious in terms of predicting good functional outcomes, Hunold said. The literature also shows that MRI's more cautious estimates are more realistic than those of PET.
"This should have therapeutic implications, especially for those high-risk patients with severely impaired function, and we think this data once more underlines the role of contrast-enhanced MRI as the new standard of reference," he said.
The project is part of a larger functional study. Only about a third of patients return for follow-up, but the results suggest that MRI has the edge in predicting functional recovery and, therefore, is better suited to revascularization planning, Hunold said in response to a question from a session moderator.
"What we know from 32 patients is that MRI was more realistic in predicting outcomes than PET but still very bad," Hunold said. "The positive predictive value was 66% for MRI and 52% for PET -- so they're both bad but MRI seems to be better."
By Eric Barnes
AuntMinnie.com staff writer
January 9, 2009
Related Reading
Adenosine stress DECT equivalent to SPECT, MRI, November 21, 2008
MRI edges out CT in postinfarct myocardial studies, May 8, 2008
Tissue Doppler beats standard echo in predicting heart failure, April 11, 2008
CTA predicts functional recovery of the myocardium, September 7, 2007
PET, SPECT measures of LVEF have superior predictive value, March 13, 2006
Copyright © 2009 AuntMinnie.com