Researchers have found that MRI with an arterial spin labeling (ASL) technique is a promising alternative to FDG-PET for tracking and diagnosing Alzheimer's disease, according to studies published online November 16 in Alzheimer's and Dementia and Neurology.
Lead study author Dr. Erik Musiek and colleagues from the Perelman School of Medicine at the University of Pennsylvania concluded that ASL-MRI may be preferred because PET requires exposure to small amounts of radioactive glucose and costs approximately four times more than the MRI technique.
Function fluctuations
"In brain tissue, regional blood flow is tightly coupled to regional glucose consumption, which is the fuel the brain uses to function," explained co-author Dr. John Detre, professor of neurology and radiology at the university, in a statement. "Increases or decreases in brain function are accompanied by changes in both blood flow and glucose metabolism."
When Alzheimer's disease is suspected, patients typically receive an MRI to detect structural changes that could indicate other causes of the disease, such as a stroke or brain tumor. ASL-MRI can be incorporated into a routine MRI scan to capture functional measures to detect Alzheimer's disease.
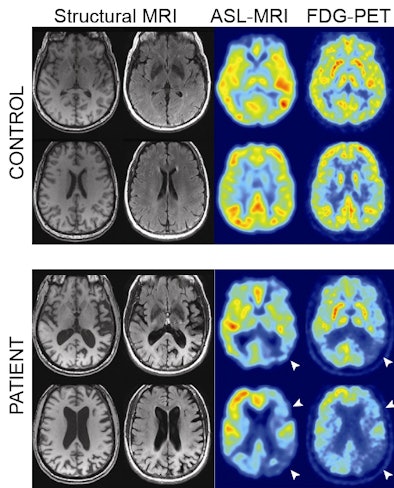 |
| Structural MRI, ASL-MRI, and FDG-PET images from control subjects (top row) and Alzheimer's patients (bottom row). All four patients were diagnosed correctly by both readers using both modalities. White arrows highlight areas of concordant hypometabolism on FDG-PET and hypoperfusion on ASL-MRI. Image courtesy of the Perelman School of Medicine. |
In the first study, published in Alzheimer's and Dementia, researchers obtained FDG-PET and ASL-MR images concurrently in 17 Alzheimer's patients and 19 age-matched control subjects. They paired the results with FDG-PET and ASL-MR images from 19 control subjects and 15 Alzheimer's patients to perform a qualitative analysis.
Both modalities revealed similar regional abnormalities in Alzheimer's disease, as well as comparable sensitivity and specificity for detecting the disease after visual review by two readers.
One reader had a sensitivity of 80% for the ASL-MR images, compared with 73% for FDG-PET. The same reader had a specificity of 95% when reading FDG-PET, compared with 89% for ASL-MRI. The second reader had a sensitivity of 60% for FDG-PET, compared with 95% for ASL-MRI. For specificity, this reader had 100% for FDG-PET and 95% for ASL-MRI.
When comparing the results between the two readers for each modality, there was 87% agreement for FDG-PET and 76% agreement for ASL-MRI. Both readers were more confident of FDG-PET reads, however.
"Although analysis of ASL-MRI images was slightly less consistent than that of FDG-PET, quantitative analysis for both modalities was nearly identical," the authors wrote. "Considering the many potential advantages of ASL-MRI, our results further bolster the potential utility of this image modality for the diagnosis of Alzheimer's disease, and reinforce the need for further efforts to standardize and validate ASL-MRI methods in larger populations of mixed neurodegenerative conditions."
In the second study, published in Neurology, ASL-MRI and FDG-PET images were compared statistically at each location in the brain by computerized analysis. Data from 15 Alzheimer's patients were compared to results in 19 age-matched healthy adults.
The patterns of reduction in cerebral blood flow were nearly identical to the patterns of reduced glucose metabolism by FDG-PET, both of which differed from the patterns of reduction in gray matter seen in Alzheimer's disease.
"Given that ASL-MRI is entirely noninvasive, has no radiation exposure, is widely available and easily incorporated into standard MRI routines, it is potentially more suitable for screening and longitudinal disease tracking than FDG-PET," the authors concluded.
If ASL-MRI were included routinely in an initial diagnostic workup, it would save the time for obtaining an additional PET scan and potentially produce a faster diagnosis, said co-author Dr. David Wolk, assistant professor of neurology and assistant director of the Penn Memory Center.
Additional studies will need to include larger sample sizes, including patients with mild cognitive impairment and other kinds of neurodegenerative conditions, according to the authors.