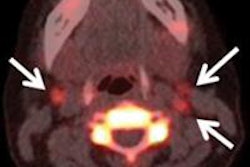
SPECT/CT changed postsurgical staging in 21% of patients with thyroid cancer, modified the treatment approach in 36% of those with the disease, and helped avoid unnecessary radiation therapy in 20% of patients with no disease in a study in the May issue of the Journal of Nuclear Medicine.
Researchers from the University of Michigan Medical Center concluded that the information from SPECT/CT helps to determine the need for radioiodine therapy or alterative options and influences long-term follow-up strategy for patient care.
Study co-author Dr. Anca Avram said SPECT/CT has substantially improved the interpretation of planar studies and can be implemented in the postoperative management protocols of thyroid cancer patients.
The findings on scans performed prior to radioiodine therapy altered the recommended sodium iodide I-131 treatment in 58% of patients, compared to therapy based on histopathologic risk stratification alone, by prescribing higher activities for treatment of regional and distant metastases and minimizing the activity prescribed for thyroid remnant ablation.
SPECT/CT is also very useful for evaluating unusual radioactivity distributions in thyroid cancer patients; accurate anatomic localization of radioactivity foci permits rapid exclusion of physiologic mimics of disease, or confirmation of metastatic lesions to unexpected sites.