Wednesday, December 4 | 11:20 a.m.-11:30 a.m. | SSK17-06 | Room S505AB
FDG-PET/MRI may offer greater lesion detection and diagnostic confidence in breast cancer cases at half the radiation dose compared with PET/CT, according to a study from NYU Langone Medical Center.FDG-PET/MRI also provided greater specificity and diagnostic confidence than whole-body MRI, the researchers found.
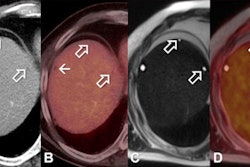
Contrast-enhanced FDG-PET/MRI provides three types of functional imaging: simultaneous mapping of increased glucose uptake, increased blood flow, and restricted diffusion typical of breast cancers and their metastases, lead researcher Dr. Amy Melsaether, an assistant professor in the department of radiology, told AuntMinnie.com.
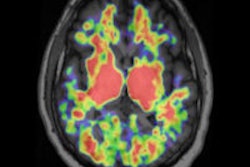
"The MRI portion of the PET/MRI provides superior tissue contrast, which, in our limited experience, helps more accurately localize areas of increased FDG uptake," she said. "High background FDG uptake in organs such as the liver and brain can obscure underlying lesions. The additional information provided by MRI can help separate abnormal PET signal due to malignancy from normal PET background signal."
In this study, 26 women with newly diagnosed stage II breast cancer and a history of metastatic disease underwent whole-body simultaneous imaging on an integrated 3-tesla PET/MRI system (Biograph mMR, Siemens Healthcare). The PET/MRI came after a PET/CT less than 120 minutes after FDG injection.
Compared with PET/CT, PET/MRI detected treatment-changing brain and bone metastases and a primary endometrial cancer in one patient each. The hybrid modality also detected additional breast cancers in two patients. Whole-body MRI detected the brain metastases and endometrial cancer, but it did not see the treatment-changing bone metastasis.
In addition, PET/MRI detected liver, bone, lung, pleural, and nodal metastases with high confidence in 17 patients in total. PET/CT saw the same lesions but with lower overall confidence, while whole-body MRI missed one patient with bone metastases and also detected metastases with lower confidence.
"The potential clinical benefits for breast cancer patients include optimized treatment based on a clearer, more accurate picture of their disease at approximately half the radiation dose of FDG-PET/CT," Melsaether said. "In particular, detection of early liver and brain metastases makes possible localized therapies, which may improve survival and quality of life."
Melsaether and colleagues plan to more closely examine the simultaneous acquisition of PET and MRI data derived from primary breast tumors.
"It is our hope that localized functional and dynamic data will eventually help predict a tumor's metastatic potential and perhaps even lead us to more individually tailored therapies, which will more aptly address the heterogeneous group of tumors under the breast cancer umbrella," she said.