British researchers are using PET imaging with the Pittsburgh Compound B (PiB) radiopharmaceutical to show -- for the first time -- increased beta-amyloid deposits in cortical gray matter and striatum regions following traumatic brain injury.
The findings could advance the understanding of traumatic brain injuries, help characterize the causes of disease progression or recovery from the incidents, potentially identify patients who are at high risk of accelerated Alzheimer's disease, and evaluate the potential benefits of antiamyloid therapies, according to the group led by Young Hong, PhD, from the Wolfson Brain Imaging Centre at the University of Cambridge.
The researchers shared their findings in an article published online on November 11 in JAMA Neurology.
Postmortem research
Recent postmortem studies have found that beta-amyloid deposits increase after a traumatic brain injury and thus accelerate the normal aging process. However, there has been an inability to quantify amyloid binding in living people, which has limited a broader understanding of beta-amyloid deposits in traumatic brain injury.
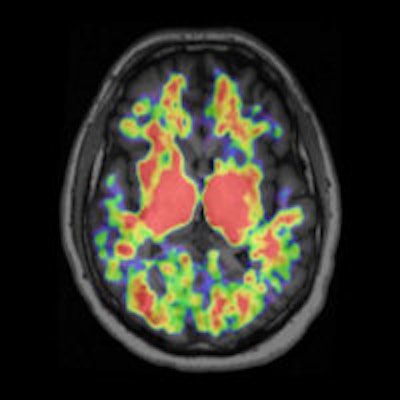
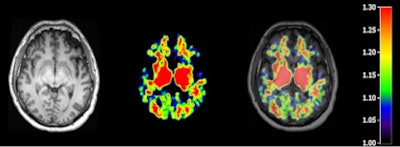 T1-weighted MR (left panel), C-11 PiB PET (middle panel), and fused image (right panel) from a patient 48 hours following severe traumatic brain injury. Image courtesy of Dr. David K. Menon, PhD.
T1-weighted MR (left panel), C-11 PiB PET (middle panel), and fused image (right panel) from a patient 48 hours following severe traumatic brain injury. Image courtesy of Dr. David K. Menon, PhD.At the same time, PET imaging techniques with several carbon-11-labeled and F-18-labeled ligands to view beta amyloid in the brain have been developed and used in Alzheimer's research. Pittsburgh Compound B, for example, is one such validated marker for cerebral amyloid deposits.
In this study, PiB-PET was performed postmortem on 15 subjects (median age, 33 years) with moderate to severe traumatic brain injury and 11 healthy controls (median age, 35 years) with no symptoms, signs, or diagnoses of neurological disease or abnormalities as shown on a brain MRI. The healthy participants also had a normal score on a mental exam.
To help segment areas of the brain into tissue classes and delineate anatomical regions of interest, participants also underwent an anatomical 3-tesla MRI scan using a Tim-Trio scanner (Siemens Healthcare).
The researchers also measured the PiB distribution volume ratio and standardized uptake value (SUV) ratio in the PET images, specifically looking at cortical gray matter, white matter, and multiple cortical and white-matter regions of interest, as well as striatal and thalamic regions of interest. Those regions of the brain are associated with executive function and memory and are likely to show early signs of Alzheimer's disease.
Amyloid presence
The analysis found that subjects with traumatic brain injury showed significantly greater PiB distribution volume ratios in cortical gray matter and in the striatum, but not in the thalamus or white matter, compared with the control group.
Increases in PiB distribution volume ratios in patients with traumatic brain injury were also seen across most cortical subregions and were replicated in SUV ratios. Control subjects, meanwhile, showed relatively low PiB binding, predominantly in the central white-matter and deep gray-matter structures.
Based on the results, the researchers concluded that PiB shows increased binding following traumatic brain injury, supported by neocortical PiB binding in regions of beta-amyloid deposits in the postmortem tissue of patients with traumatic brain injury.
"PiB-PET could also help us in identifying the proportion of patients with moderate to severe traumatic brain injury who do show amyloid deposits, and in exploring whether any patients with mild traumatic brain injury show such deposition because postmortem evidence is unavailable for this latter group," the authors wrote.
Hong and colleagues cited several limitations of their study, including the small study cohort. Perhaps most important, they noted, although the data are concordant with previous postmortem studies that evaluated amyloid deposits in traumatic brain injuries, the small proportion of late studies in this 15-patient cohort "limits inferences regarding the temporal pattern of PiB binding in vivo and requires confirmation in a larger cohort."
Future studies could also use PiB-PET to follow the course of beta-amyloid accumulation following traumatic brain injury in a way that cannot be done in postmortem studies, and possibly determine if beta amyloid reoccurs decades after the traumatic brain injury, the authors suggested.
"Such an approach would also allow for the analysis of beta-amyloid deposits in traumatic brain injury in the context of cognitive function and host genotype (particularly [apolipoprotein E]), which were not addressed in the present study," Hong and colleagues wrote.