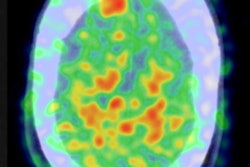
PET scans with Pittsburgh Compound B (PiB) showed a dramatic increase in brain beta-amyloid deposits in older adults with no signs of dementia, and there was also a strong association between arterial stiffness and beta amyloid, according to a study published online March 31 in the Journal of the American Medical Association.
The results "add a new dimension to our understanding of the intersection of arteriosclerosis, brain health, and [beta-amyloid] deposition in nondemented older adults," the authors wrote.
In the study, the number of individuals positive for beta-amyloid deposits increased from 48% at baseline PiB-PET scans to 75% at follow-up two years later. During the same two-year period, the amount of beta-amyloid deposits in the brain increased in 90% of the cohort of nondemented adults (JAMA, March 31, 2014).
"One of the big 'take-home' messages is that amyloid deposition is not just a factor in Alzheimer's disease, [and] that these older adults without dementia have a lot of amyloid," lead author Timothy Hughes, PhD, a postdoctoral scholar in the department of internal medicine at Wake Forest School of Medicine, told AuntMinnie.com.
 Timothy Hughes, PhD, from Wake Forest School of Medicine.
Timothy Hughes, PhD, from Wake Forest School of Medicine.
In addition, increases in central arterial stiffness were linked with increases in beta-amyloid deposition over the two years, the researchers found.
"We're not exactly sure how it causes amyloid or whether or not there is sort of an underlying factor between arterial stiffness and amyloid that we can't measure," Hughes said. "We already know that arterial factors are related to brain health, but this adds that extra dimension and says they also are related to amyloid. So we need to look at this relationship in more detail."
Beta-amyloid connection
The study is a follow-up of earlier research by Hughes and colleagues in which 91 dementia-free people between the ages of 83 and 96 years underwent brain MRI and PiB-PET scans in 2009. Then, in 2011, the researchers measured resting blood pressure, mean arterial pressure, and arterial stiffness by pulse wave velocity using a noninvasive and automated waveform analyzer (Neurology, November 5, 2013, Vol. 81:19, pp. 1711-1718).
Of those 91 participants, 44 (48%) were beta-amyloid-positive on PET scans, and beta-amyloid deposits were associated with mixed pulse wave velocity, systolic blood pressure, and mean arterial pressure. One standard deviation increase in brachial-ankle pulse wave velocity doubled the odds of being positive for beta amyloid. High white-matter hyperintensity burden was associated with increased central pulse wave velocity, systolic blood pressure, and mean arterial pressure.
They concluded that arterial stiffness was associated with beta-amyloid plaque deposition in the brain, regardless of blood pressure and apolipoprotein E (APOE) genotype, which has been identified as a genetic risk factor for Alzheimer's. Individuals with both high beta-amyloid deposition and white-matter hyperintensities, which are also considered contributors to dementia, had the most arterial stiffness.
The current study included the same patients, but with a second round of assessment. From July 2010 through November 2012, 81 of the participants who remained nondemented returned for a second set of scans. Mean follow-up time between the PiB-PET scans was 1.8 years, the authors wrote.
Arterial stiffness
Arterial stiffness is a natural process that occurs with aging. Arteries normally are very elastic, but the increased pressure of blood flow over time leads to arterial stiffness.
For pulse wave velocity, the researchers measured the pulse at two points on the body, calculating the time it takes a heartbeat to get to those two points. "The greater the speed, the stiffer the artery," Hughes explained. "You want those central arteries to slow that pulse wave velocity down. Once you lose that ability, then it is up to the rest of the vasculature to accommodate that increased pressure."
In the study, the researchers measured pulse wave velocity in the central (carotid-femoral and heart-femoral velocity), peripheral (femoral-ankle velocity), and mixed (brachial-ankle velocity) vascular beds. Hughes said the current study is unique in that they took pulse wave velocity measurements at different artery beds.
"We did that because it tells us different things about the whole extent of the arteries," he said. "The carotid-femoral [pulse wave velocity] is the gold standard for measuring central pressure, or central arterial stiffness ... but there are other arteries involved in arterial stiffness as well."
Follow-up results
The number of beta-amyloid-positive individuals increased from 48% (44 of 91 patients) at baseline to 75% (61 of 81 patients) at follow-up two years later, Hughes and colleagues found.
In addition, brachial-ankle pulse wave velocity was significantly higher among beta-amyloid-positive participants at baseline and follow-up, while femoral-ankle pulse wave velocity was higher among beta-amyloid-positive participants at follow-up.
Each standard deviation increase in brachial-ankle pulse wave velocity was associated with a fourfold increase in the odds of a person being beta-amyloid positive at follow-up, compared with the twofold increase seen at baseline.
The accumulation of beta-amyloid over time was significantly associated with greater measures of central arterial stiffness, as well as a history of cardiovascular disease and carrying the APOE4 allele, according to the authors.
"These findings confirm and extend our initial results showing that beta-amyloid deposition is strongly related to the severity of peripheral vascular stiffness and that this relationship differs by arterial bed measured," they wrote. "Taken together, the results from these two studies show that the degree of systemic arterial stiffness, measured by [brachial-ankle pulse wave velocity], is strongly associated with the extent of [beta-amyloid] deposition at both baseline and follow-up."
"In contrast, measures of central stiffness ... are more strongly associated with the progression of [beta-amyloid] accumulation in the brain over time," they continued.
Hughes said they were surprised to find that 45% of the cohort was beta-amyloid positive in the baseline scan, and that the percentage increased to 75% only two years later.
Also, while they knew from the first study that there was a relationship between arterial stiffness and beta amyloid, Hughes said he was surprised "how strong it was at both time points at baseline and follow-up, and that arterial stiffness was related to [beta-amyloid] progression over time."
"Oftentimes, we hope to see something as clean as this, but I think it really underscores the fact that we might have a good indicator of brain amyloid here, in that it holds up over time," he said.
Hughes and colleagues next plan to focus on a younger cohort in their 50s and 60s. "Those individuals with hypertension might show amyloid earlier; that is something that we would like to do and, obviously, replicate these findings in any age group," he said.
Previous studies have found that some people show clinical signs of beta-amyloid accumulation in their 40s. "So finding modifiable risk factors for brain amyloid deposition will not only impact Alzheimer's disease prevention, it will also contribute to healthy brain aging," Hughes said.