Compared to PET/CT, FDG-PET/MRI with a fully integrated whole-body scanner is "technically and clinically robust" in its evaluation of bone lesions, despite differences in attenuation correction between the two hybrid modalities, according to a study in the February issue of the Journal of Nuclear Medicine.
German researchers say their findings could be beneficial for patients with primary bone tumors, early bone marrow infiltration, and tumors with low uptake on PET. Based on the results, they also recommend T1-weighted turbo spin-echo (TSE) MRI as a routine protocol for oncologic PET/MRI.
The study's lead author is Dr. Matthias Eiber from the department of radiology at Technische Universität München (JNM, February 2014, Vol. 55:2, pp. 191-197).
An edge in soft-tissue contrast
Previous research has shown that whole-body integrated PET/MRI can evaluate bone lesions better than PET/CT due to MRI's greater soft-tissue contrast, Eiber and colleagues wrote. However, unlike attenuation correction with PET/CT, PET/MRI "ignores the contribution of cortical bone in the attenuation map," they noted.
The U.S. Food and Drug Administration (FDA) has only approved a two-point Dixon-based MRI sequence for attenuation correction with a whole-body fully integrated PET/MRI system.
"This [Dixon-based] approach neglects the contribution of bone signal," the authors wrote. To date, there is "no convincing clinical data showing whether it is necessary to additionally segment bone in MR attenuation correction maps."
Thus, Eiber and colleagues sought to determine the potential of PET/MRI with two diagnostic imaging sequences for the detection and characterization of bone lesions, compared with PET/CT. They also wanted to analyze the significance of neglecting the contribution of bone in Dixon-based attenuation correction.
Imaging protocols
The retrospective study included 119 patients (65 men, 54 women; mean age, 53.4 years) who were referred for indications including head and neck, breast, thyroid, and gastrointestinal cancers and sarcoma.
All subjects underwent a single-injection, dual-imaging protocol using FDG on a PET/CT scanner. They also received a subsequent PET/MRI scan with a T1-weighted volumetric interpolated breath-hold examination (VIBE) Dixon sequence for attenuation correction, as well as an unenhanced coronal T1-weighted turbo spin-echo (TSE) sequence for bone analysis.
"T1-weighted spin-echo sequences usually have a higher in-plane resolution and provide a better visualization of bone marrow and bone lesions than the T1-weighted Dixon VIBE sequence used for attenuation correction in PET/MRI," the authors wrote.
Patients fasted for six hours before receiving an injection of approximately 382 MBq of FDG (range, 193-504 MBq), depending on body weight. PET/CT scans were performed first (Biograph Sensation 64, Siemens Healthcare), followed by PET/MRI on a fully integrated whole-body hybrid system (Biograph mMR, Siemens) at a mean 137.2 minutes after FDG injection. The average time between the start of the two exams was 49.6 minutes.
Eiber and colleagues divided the results into three sets of images, which were analyzed by two experienced readers:
- Set A included CT images together with PET from PET/CT.
- Set B included T1-weighted VIBE Dixon images with PET from PET/MRI.
- Set C included T1-weighted TSE images with PET from PET/MRI.
The images were rated on a four-point scale for lesion detection, with 0 meaning no uptake on PET or a PET-negative lesion and 3 denoting high FDG uptake. Each PET-positive lesion was also rated on a four-point scale for delineation, with 1 meaning no delineation possible and 4 indicating excellent delineation. Characteristics and severity of each lesion were ranked on a five-point scale, with 1 as definitely malignant and 5 as definitely benign.
Lesion detection
There were 98 conspicuous lesions (90 malignant, eight benign) in 33 of the 199 patients, according to the authors. All 98 lesions were identified on PET/CT (set A) and on the T1-weighted TSE sequence for PET/MRI (set C). The T1-weighted VIBE Dixon sequence (set B) missed one PET-negative malignant lesion in the ribs.
In pinpointing the location of the lesions, T1-weighted TSE (mean rating, 2.84 ± 0.42) performed significantly better than both CT (mean rating, 2.57 ± 0.54) and T1-weighted VIBE Dixon (mean rating, 2.57 ± 0.54).
Of the 98 lesions, 85 (87%) showed abnormally increased uptake on PET. Visual lesion conspicuity on PET was similar for both hybrid modalities, with a mean 2.82 ± 0.45 for the PET dataset from PET/CT and 2.75 ± 0.51 for the PET results with PET/MRI.
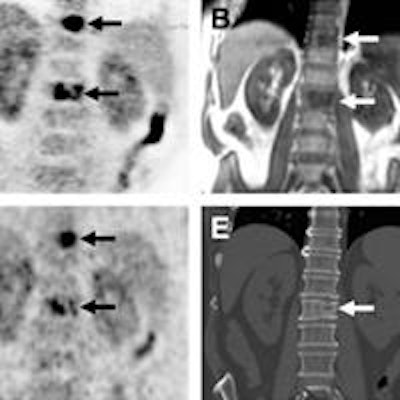
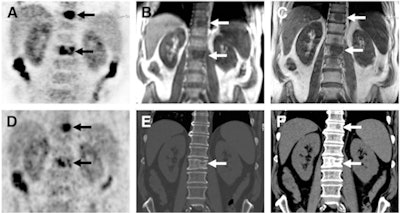 Images of bone metastases (arrows) in a 69-year-old man presenting for staging of oropharyngeal cancer: PET/MRI with coronal PET (A), coronal T1-weighted Dixon MRI sequence (B), and coronal T1-weighted TSE MR sequence (C). PET/CT scan includes coronal PET (D) and coronal bone (E) and soft-tissue CT (F). Two metastases in spine show intense uptake in both PET datasets (A and D). Replacement of bone marrow is seen in both T1-weighted Dixon MRI sequence (B) and T1-weighted TSE MR sequence (C), with better lesion delineation in TSE than in VIBE Dixon because of higher in-plane resolution. Faint sclerosis is present as anatomic correlate of caudal metastases in both bone window (E) and soft-tissue window (F) on CT, whereas cranial metastasis is depicted only in soft-tissue image. Images courtesy of JNM.
Images of bone metastases (arrows) in a 69-year-old man presenting for staging of oropharyngeal cancer: PET/MRI with coronal PET (A), coronal T1-weighted Dixon MRI sequence (B), and coronal T1-weighted TSE MR sequence (C). PET/CT scan includes coronal PET (D) and coronal bone (E) and soft-tissue CT (F). Two metastases in spine show intense uptake in both PET datasets (A and D). Replacement of bone marrow is seen in both T1-weighted Dixon MRI sequence (B) and T1-weighted TSE MR sequence (C), with better lesion delineation in TSE than in VIBE Dixon because of higher in-plane resolution. Faint sclerosis is present as anatomic correlate of caudal metastases in both bone window (E) and soft-tissue window (F) on CT, whereas cranial metastasis is depicted only in soft-tissue image. Images courtesy of JNM.As for characterizing the lesions, the researchers found no significant differences between the three image sets. Of the 90 malignant lesions, 85 were correctly classified in set A, 84 in set B, and 86 in set C.
In addition, six PET-negative lesions were correctly classified as malignant bone lesions in the PET/CT and T1-weighted TSE images. Of those lesions, one was completely missed by the T1-weighted VIBE Dixon sequence in PET/MRI, but it was correctly recognized in the other two sets as malignant.
Among the bone lesions and 630 regions of normal bone, the mean standardized uptake values (SUVs) for PET/CT (R = 0.917) and PET/MRI (R = 0.950) also correlated significantly.
Clinical relevance
In terms of location and delineation of PET-positive bone lesions, the T1-weighted TSE MRI sequence performed significantly better than CT or the T1-weighted VIBE Dixon sequence, Eiber and colleagues concluded.
PET from PET/MR was equivalent to PET from PET/CT regarding FDG uptake assessed visually. "Consequently, the attenuation correction provided by the T1-weighted VIBE Dixon sequence, which neglects the contribution of cortical bone, is adequate for clinical use," they wrote. "In our study, this adequacy is expressed by only slight differences in the visual lesion conspicuity between the two PET datasets."
"However, the higher rate of concordant findings between T1-weighted TSE images and PET compared with CT and Dixon in-phase images can potentially improve diagnostic certainty, and its inclusion in an oncologic PET/MR protocol is recommended," they added.
Eiber and colleagues recommended that larger prospective studies in the future include both FDG-avid and FDG-negative malignancies to "further evaluate the role of PET/MRI for a broad variety of bone lesions, including FDG-negative tumors."