
At many large hospitals, radiologists are increasingly using MRI to obtain second opinions on ambiguous fetal ultrasound scans, according to a growing litany of case reports.
Based on their success, researchers believe the modality can help direct the course of many pregnancies. But they caution that prenatal MRI is best left to radiologists familiar with the technique, and that it’s needed only in the most difficult-to-interpret ultrasound cases.
An example of MRI’s newfound obstetric niche can be found at New York City’s Mount Sinai School of Medicine, where radiologists often use the modality to better image cranial masses that are difficult to diagnose solely with ultrasound, according to a report presented at the 2001 American Institute of Ultrasound in Medicine meeting.
In one case, ultrasound appeared to portray a fetus’s skull as perforated by blood vessels -- a potentially fatal anomaly, explained Dr. Carl Saphier, director of labor and delivery at Mount Sinai. Fortunately, on closer inspection using MRI, the skull was found to be intact.
 |
There are several reasons why MRI outperforms ultrasound, said Saphier, who each month sends about ten pregnant women out of a thousand to MRI. First, ultrasound is limited by amniotic fluid; sound waves need water to pass through, and when fluid levels are low, image quality suffers.
Second, surgical material and excessive fatty tissue often disrupt sound waves. This was the case for one patient at Mount Sinai. An ultrasound of a morbidly obese woman, who had also undergone abdominal mesh placement to repair a hernia, suggested that her fetus might have an encephalocele, a disorder in which there is a gap in the skull. But the image wasn’t conclusive.
 |
"The sound waves couldn’t penetrate the abdominal wall of the obese patient," Saphier said. "But the MRI did quite well. It confirmed the suspected anomaly and the pregnancy was terminated."
In addition to cranial masses, Saphier and colleagues have also used MRI’s exquisite resolution to obtain better fetal images of diaphragmatic hernias, kidneys, and brain abnormalities.
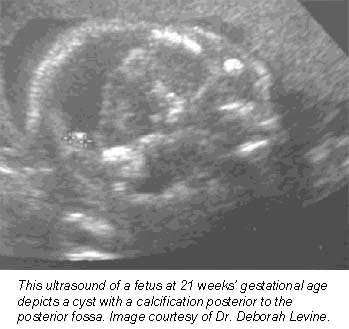
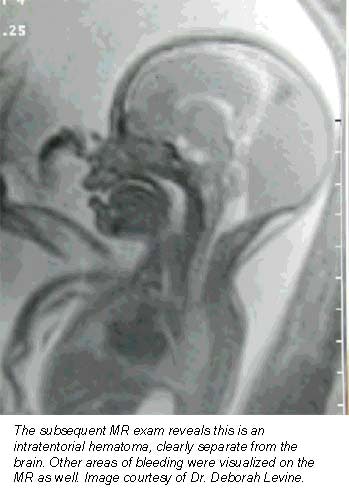
Still more applications are being pioneered at Boston’s Beth Israel Deaconess Medical Center, where researchers are nearing the end of a five-year study funded by the National Institutes of Health to evaluate how MRI complements prenatal ultrasound in the diagnosis of central nervous system disorders. So far, their results are promising.
"MR almost always will make you more sure of your diagnosis," said associate professor of radiology Dr. Deborah Levine. "It informs how we counsel the patient. Sometimes it directs the mode and timing of delivery, or helps a patient decide whether to terminate a pregnancy."
Levine, who oversees about one prenatal MRI exam per week, said she finds the modality especially helpful in determining whether fetuses suffer from central nervous system anomalies, as well as for defining many chest masses. Some radiologists are also using MRI to get a better idea of fetal volume, particularly in abnormal fetuses that are either too large or too small, she said.
Basically, MR is helpful whenever ultrasound is unclear, Levine said -- a general rule of thumb that’s allowed the procedure to catch on at institutions nationwide.
In Europe, according to a Dutch study published in Fetus Diagnosis and Therapy, researchers from the University Hospital Amsterdam used ultrafast MRI, which enables scanning without sedating the fetus, to image 39 patients with 41 fetuses in whom ultrasound showed a suspicion of brain, spine, or skeletal abnormalities. MRI offered additional information in 22 of the fetuses, leading the researchers to conclude that MRI is advisable in cases that appear equivocal on ultrasound (November-December 2000, Vol.15:6, pp.364-372).
But don’t look for MRI to usurp ultrasound. Despite the advantages of MRI, ultrasound is still inexpensive, pervasive, and easy to use -- so it will remain the standard prenatal imaging test, Saphier said. The ultrasound transducer can be easily maneuvered to obtain quick, quality images, he said.
Except for ultrafast protocols, MRI is limited by fetal movement, he added. Levine pointed out that although fetal MRI has proven itself clinically, its cost-effectiveness is still being examined -- a task made difficult because prenatal MR often occupies a difficult-to-quantify gray area: It makes radiologists more confident of a diagnosis, but in many cases doesn’t affect patient management.
And fetal MRI is tricky. It should only be used clinically at centers that have experience with MRI and pregnancy, Saphier said. At Mount Sinai, Saphier pools together everyone’s expertise when cases are sent to the MR room. Obstetricians collaborate with radiologists, and both interpret the scans.
"I would reserve MRI only for those cases that need to be confirmed because the ultrasound isn’t clear," he said.
All this means that ultrasound will remain the primary modality for prenatal diagnosis. But at centers that have the know-how and resources, Saphier believes MRI will give radiologists a powerful recourse when they’re faced with puzzling ultrasound scans.
By Dan KrotzAuntMinnie.com contributing writer
April 25, 2001
Related Reading
MRI's new role: assessing obscure fetal abnormalities, December 3, 1999
Click here to post your comments about this story. Please include the headline of the article in your message.
Copyright © 2001 AuntMinnie.com




















