Cerebral microvasculopathy could be an underlying mechanism for cognitive dysfunction, based on MR studies performed in patients with antiphospholipid syndrome (APS), according to Greek investigators.
APS, broadly defined as the presence of arterial or venous thromboses associated with antiphospholipid (aPL) antibodies, often occurs in conjunction with systemic lupus erythematosus (SLE). This thrombosis can occur at any vascular site and in any organ system, said Dr. Maria Tektonidou from the department of pathophysiology at the National University of Athens School of Medicine and the Athens-based Euroclinic Hospital.
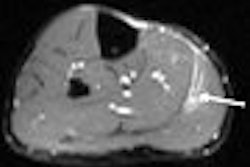
"Abnormal MRI findings in APS include single or multiple infarcts, white-matter lesions (WMLs), cortical atrophy, and focal hemorrhage," they wrote. For this cross-sectional study, 60 patients with definitive APS and 60 healthy volunteers were enrolled (Archives of Internal Medicine, November 13, 2006, Vol. 166: 20, pp. 2278-2284).
The APS patients were divided into two groups: those with central nervous system (CNS) involvement and those who had never had a neuropsychiatric event. The gadolinium-enhanced MR protocol included sagittal and axial spin-echo T1-weighted images, axial spin-density T2-weighted images, and proton-density, fluid-attenuated inversion-recovery images on a 1.5-tesla scanner. Co-author and radiologist Dr. Grigorios Kotoulas read the images.
"Infarcts were defined as focal lesions with increased signal intensity on T2-weighted images and reduced signal intensity on T1-weighted images," the authors explained. "White-matter lesions on MRI were identified as ill-defined hyperintensities on T2-weighted and proton-density, fluid-attenuated inversion-recovery images without prominent hypointensity on T1-weighted images. We classified WMLs according to their location (and) to their size as punctuate."
According to the results, a significant association was found between the presence of WMLs on MRI and livedo reticularis, a dermatologic manifestation of APS characterized by diminished blood flow in the arterioles and dilation of venules and capillaries.
In addition, a significant association was found between cognitive deficits and small periventricular, as well as subcortical, WMLs, particularly in patients with no CNS involvement. Specifically, 88% of the patients with WMLs and no CNS symptoms had cognitive deficits versus 21% without WMLs.
"The absence of any association between cognitive abnormalities and a history of CNS involvement is of particular interest," the authors wrote. "The pathogenesis of WMLs remains unknown, but it is generally thought that WMLs are related to vascular disease in the long penetrating arteries of the brain."
Finally, no association was found between cognitive deficits and brain infarcts on MRI. The results help to broaden the range of neurological manifestations found in APS, the authors stated.
By Shalmali Pal
AuntMinnie.com staff writer
January 3, 2007
Related Reading
MRI spots white-matter changes in movement disorder patients, November 24, 2006
Asymptomatic left carotid artery stenosis linked to cognitive decline, May 11, 2001
Copyright © 2007 AuntMinnie.com



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)