By combining functional MRI (fMRI) and passive speech stimulation, researchers at Columbia University Medical Center in New York have discovered physiologic differences between autistic and healthy children, according to a study in the August issue of Radiology.
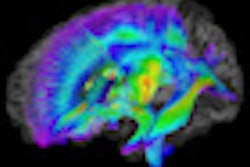
Functional MR images of the superior temporal gyrus and primary auditory cortex of the brain, which are associated with sentence comprehension, demonstrate the "potential utility of fMRI as an objective indicator of language impairment in autism," wrote a research team led by Grace Lai, PhD, of Columbia's Functional MRI Research Center.
Autism is often detected by parents and clinicians who notice when young children do not reach certain milestones in their early development, the authors noted. Given that fMRI can be performed with no great risk or invasiveness compared to other imaging modalities, "functional imaging of impaired systems, including language, may appropriately aid objective indications of language impairment in autistic patients," they wrote.
Study participants
The prospective analysis included data acquired between 2008 and 2010 from a study designed to investigate neural mechanisms that may cause language impairment in autistic children. The researchers enrolled 15 healthy, nonautistic subjects (mean age, 12.1 years) as the control group, in addition to 12 autistic subjects (mean age, 12.4). All subjects were imaged while alert (Radiology, August 2011, Vol. 260:2, pp. 521-530).
The study also evaluated an additional 27 autistic children (mean age, 8.6 years) who received routine structural and functional MRI scans while sedated.
The autistic participants were diagnosed with the condition via criteria from the Diagnostic and Statistical Manual of Mental Disorders and the Autism Diagnostic Interview-Revised (ADI-R). A child is considered autistic when his or her ADI-R score is greater than a specified minimum in three categories: a social score greater than 10, a language score greater than 8, and repetitive behavior rating greater than 3.
The researchers excluded healthy and autistic individuals with comorbid neurologic or developmental disorders, as well as those with contraindications to MRI. In addition, control subjects were eliminated from the research if they were diagnosed with any psychiatric conditions or were taking psychiatric medications.
MRI scans were conducted on a 1.5-tesla system (Twin Speed, GE Healthcare), with fMR images acquired by using an echo-planar T2-weighted gradient-echo sequence.
The researchers also prerecorded the voices of the children's parents, asking the parents to talk about the same topics, such as being in the imaging unit, recent events, or plans after the MRI procedure. Children listened to the words through MRI-compatible headphones.
"Familiar voices are used to increase task compliance in younger and autistic children," Lai and colleagues noted in the study.
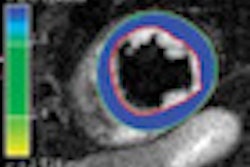
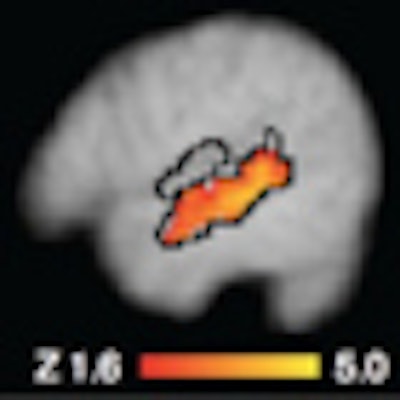
As part of the analysis, the group also measured the spread and amplitude of blood oxygen level-dependent (BOLD) activation within certain regions of interest of the primary auditory cortex and superior temporal gyrus. To quantify the difference between individual autistic and healthy children, those with standard measures of less than 1.0 from the control group's mean were considered positive for autism, while those with values above that mark were considered negative for autism.
Results
Upon analysis of the functional MR images and measurements, Lai and colleagues found that activity in the primary auditory cortex did not differ between the autistic children and the healthy control subjects. However, they did see a difference in mean amplitude and spread of activity in the superior temporal gyrus between autistic and healthy children (p = 0.001).
Among 10 (83%) of the 12 autistic children who were not sedated, the researchers noted a decrease of at least one standard deviation below the level of the healthy group.
All autistic children also scored in the high range of impairment on all three ADI-R categories. Reciprocal social interaction had a mean of 21.18, language and communication had a mean of 18.87, and restricted, repetitive, and stereotyped behavior registered a mean of 6.0.
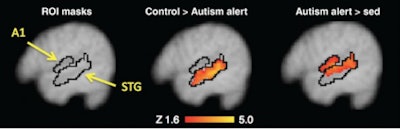 |
| MR image (left) illustrates anatomic regions of interest for the primary auditory cortex and superior temporal gyrus. Activation maps (middle and right) show greater activity within the superior temporal gyrus but not the auditory cortex in the control group compared with the nonsedated autism group, and greater activation within both the superior temporal gyrus and auditory cortex in the nonsedated subjects compared with the sedated autism group. Image courtesy of Radiology. |
Lai and colleagues did not measure ADI-R scores in the healthy control subjects, surmising that the healthy children would have scored zero.
ADI-R scores for language or repetitive behaviors among the sedated and nonsedated autistic groups did not differ significantly, and sedated children were more impaired relative to social interaction.
Study limitations
The authors cited several limitations to the study, including age and how these results would apply to younger children, "who are at an age at which an objective medical diagnostic procedure would be most useful for the purpose of early intervention."
They also noted that the study did not include subjects with abnormalities other than autism, so "our findings cannot be used to differentiate autism from other causes of developmental delay."
However, based on the findings, the group did conclude that functional MRI activation within the superior temporal gyrus in response to passive speech stimulation "helped differentiate autistic from control subjects, demonstrating the potential utility of functional MRI as an objective indicator of language impairment in autism."
Lai and colleagues recommended that future research include patients with varying levels of autism to help establish a relationship between the measures within the current study.
"If so, functional MR imaging may serve as a neural measure of change in function following medical or neuropsychologic intervention," they added.