Researchers at the University of California, San Diego (UCSD) have developed a new MRI technique that shows early promise for noninvasively detecting and evaluating nonalcoholic fatty liver disease (NAFLD) in children, according to a study published online February 5 in Hepatology.
The technique, known as magnitude-based MRI, is designed to estimate liver proton density fat fraction, a biomarker of liver fat content. And while it eventually might offer an alternative to invasive liver biopsy to diagnose young patients with liver disease, the researchers cautioned that MRI "is not yet sufficient to replace liver biopsy in children."
Still, depending on how the new MRI technology is used, they estimated that it could correctly classify between 65% and 90% of children as having or not having fatty liver tissue.
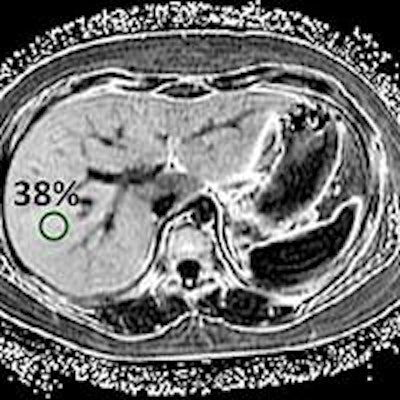
NAFLD is characterized by fat deposits in at least 5% of a child's liver cells, whereas the normal fat level is 1%. The disease can be exacerbated by obesity and diabetes and lead to hepatitis, cirrhosis, and liver cancer.
Currently, diagnosing NAFLD requires a liver biopsy to determine the presence and severity of liver fat, based on the percentage of liver cells that contain fat droplets. Lead author Dr. Jeffrey Schwimmer, professor of clinical pediatrics at UCSD and director of the Fatty Liver Clinic at Rady Children's Hospital, noted that conventional liver biopsy can result in both misdiagnoses and missed diagnoses.
Schwimmer and colleagues prospectively compared the MRI technique with a standard liver biopsy in 174 children (mean age, 14 years; range, 8-17 years). The cohort included children who had liver biopsies and showed no signs of fat deposits, as well as young patients with biopsy-proven NAFLD (Hepatology, February 5, 2015).
Each patient underwent a 3-tesla MRI scan to estimate liver proton density fat fraction. The mean time between the MRI and liver biopsy was 57 days (± 51 days). The MRI results were compared with pathology from the conventional liver biopsy.
The researchers found a strong correlation (0.72) between the amount of liver fat measured by the new MRI technique and the degree of liver fat determined by pathology. The correlation was stronger among girls (0.86) than boys (0.70), and it was weaker in patients with stage 2 to 4 fibrosis (0.61) than in children with no fibrosis (0.76) or stage 1 fibrosis (0.78).
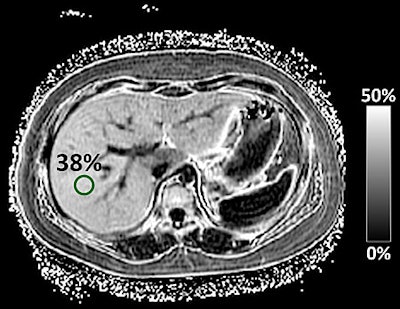 MR image of a child’s liver with severe NAFLD. The liver is 38% fat, compared with a normal level of 1%. Image courtesy of UCSD School of Medicine.
MR image of a child’s liver with severe NAFLD. The liver is 38% fat, compared with a normal level of 1%. Image courtesy of UCSD School of Medicine.Using threshold values of 0.69 to 0.82 to distinguish between no fat concentration and mild fat concentration in the liver, the MRI-estimated liver proton density fat fraction was able to predict the histologic degree of fat concentration with an overall accuracy of 56%.
However, no single threshold "had sufficient sensitivity and specificity to be considered diagnostic for an individual child," according to the researchers.
Therefore, while MRI has "sufficient potential clinical utility in the evaluation of NAFLD," the modality is "not yet sufficient to replace liver biopsy in children," Schwimmer and colleagues wrote. "How to best integrate MRI into clinical protocols and whether MR-based techniques such as MR elastography may be synergistic with MRI-estimated liver [proton density fat fraction] for the assessment of NAFLD need to be prospectively evaluated."
Despite the caution, the researchers described the findings as an important step toward using the MRI technique effectively, given the correlation between a patient's gender and the amount of scarring in the liver from NAFLD.