Diffusion-weighted imaging (DWI) derived from MRI can help reduce unnecessary biopsies in breast cancer screening, according to presentations given May 9 at the annual meeting of the International Society for Magnetic Resonance in Medicine (ISMRM).
In two presentations, Debosmita Biswas from the University of Washington Medical Center in Seattle and Dr. Rie Ota from Kyoto University in Japan showed abstracts from their teams' research showing the benefits of diffusion-weighted imaging.
"Breast diffusion-weighted imaging can be successfully and safely integrated with breast MR clinical interpretations to reduce biopsies," Biswas said.
ISMRM is holding this week's meeting in conjunction with the European Society for Magnetic Resonance in Medicine and Biology and the International Society for MR Radiographers and Technologists.
An alternative to contrast-enhanced MRI?
Dynamic contrast-enhanced MRI is high in sensitivity, but also has lower specificity, leading to unnecessary biopsies. DWI has shown promise in supplemental imaging in recent years without the use of contrast agents, including increasing specificity.
In her presentation, Biswas talked about using DWI in validating thresholds established in a 2019 study by Rahbar et al in Clinical Cancer Research that showed a potential reduction of nearly 21% in biopsies. The team also wanted to compare diagnostic performance using commercially available versus research software tools.
The researchers looked at data from high-risk women who underwent breast cancer screening. These included a total of 101 lesions (78 benign, 23 malignant) from 86 women. Readings of BI-RADS 4 and 5 from MRI scans and biopsy recommendations were included. The team looked at both prospective and retrospective data, as well as data from an offline approach that replicated that of the 2019 study.
The study authors found that their prospective approach, in which data was collected at the time of interpretation by the attending radiologist, showed that DWI-MRI achieved statistical significance in differentiating between benign and malignant lesions and yielded the highest performance. This included an area under the curve (AUC) of 0.66.
While the prospective method had slightly lower sensitivity and lower biopsy reduction than the retrospective and offline approaches, Biswas said the results support DWI use in practice since results were close to the 2019 study.
"We saw comparable performance of using clinical PACS workstations versus custom research tools," she said.
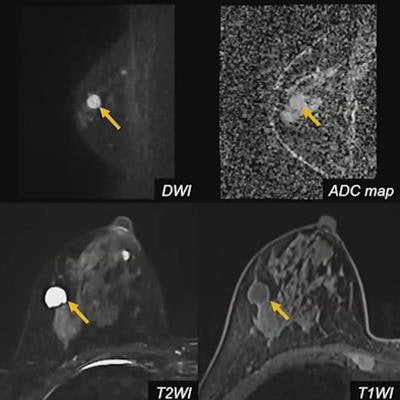
But going deeper, modifying BI-RADS through high-resolution DWI could be helped by weighted MRI sequences. This is what Ota's presentation focused on.
The Ota team wanted to add noncontrast sequences from MRI, such as T1- and T2-weighted imaging combined with diffusion-weighted imaging and test this approach's performance.
They looked at data from a total of 98 lesions (60 malignant, 38 benign) from 98 women with an average age of 55 years. Two experienced readers categorized lesions based on the modified BI-RADS and categories were compared to pathological diagnosis.
For the modifications, BI-RADS 4 lesions were divided into three subcategories depending on the likelihood of malignancy: 4A, which had a 2% to 10% likelihood; 4B, which had a 10% to 50% likelihood; and 4C, which had a likelihood of 50% to 95% or higher.
 Noncontrast sequences from MRI, such as T1- and T2-weighted imaging, could further help diffusion-weighted breast imaging, according to research presented May 9 at ISMRM 2022.
Noncontrast sequences from MRI, such as T1- and T2-weighted imaging, could further help diffusion-weighted breast imaging, according to research presented May 9 at ISMRM 2022.The readers were comparable in their respective analyses. They had an average sensitivity of 79.15% and an average specificity of 89.45%. The researchers also found that apparent diffusion coefficient (ADC) measurements were significantly lower among malignant lesions (p < 0.001).
Ota said this approach to high-resolution DWI allowed for detailed morphological evaluation similar to contrast-enhanced MRI and enabled radiologists to evaluate lesions with "excellent" performance.
"Associated features [ADC, size, etc.] contributed to upgrade suspicious lesions and improve diagnostic performance," she said.
So, what's holding DWI-MRI from being used more regularly in breast imaging? Biswas said that image resolution has generally lower resolution than dynamic contrast-enhanced imaging.
"I guess radiologists are more used to seeing beautiful dynamic contrast images and even now, the resolution of diffusion-weighted imaging is not as great," she said.
However, she added that with training, radiologists could look at ADC values than currently.