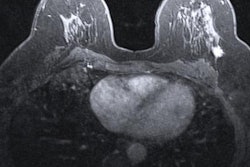
Preoperative MRI is tied to reduced risk of breast cancer recurrence in patients aged 50 years or younger with cancer diagnosis and for hormone receptor-negative cancers, research presented December 1 at the RSNA annual meeting found.
In her talk, Dr. Heera Yoen from Seoul National University Hospital in South Korea presented her team's findings, which suggest that MRI could be beneficial in terms of recurrence outcomes.
"Our results may support the usefulness of preoperative MRI in young breast cancer patients and support tailored MRI utilization," Yoen said.
Breast cancer in young women is typically more advanced and exhibits more aggressive behavior. Previous research shows that cancer in this area has worse mortality and morbidity outcomes.
Yoen said this is because there was previously less concern for cancer risk in younger populations, as well as no standardized guidelines for screening compliance. Along with that, screening mammography has less sensitivity in dense breast tissue.
The jury is out on preoperative breast MRI in younger women when it comes to long-term survival outcomes. While proponents suggest MRI can improve surgical outcomes, recurrence, and survival rates, critics say there is not enough data to support this.
Yoen and colleagues wanted to explore and compare the effect of preoperative MRI on recurrence and survival outcomes in young women with breast cancer diagnoses. They also looked at the interaction between preoperative MRI and breast cancer hormone receptor status.
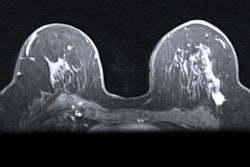
The researchers reviewed data collected from 2012 to 2015 from 1,778 patients. Out of these, 1,653 patients (93%) had undergone MRI and 125 patients (7%) did not. They matched and balanced patients without preoperative MRI with women who had preoperative MRI.
On a median follow-up of seven years, the researchers reported that the cumulative cancer recurrence rate was 7% (n = 105). Eleven of these cases (9%) came from the non-MRI group while 94 cases (6%) came from the MRI group. The team found a significant association in the matched cohort between MRI and a lower risk of total recurrence; the group of patients who had received preoperative MRI had a hazard ratio (HR) of 0.4 for total recurrence compared with the control group (p = 0.018).
Also, patients who received MRI had a significantly higher recurrence-free survival rate (95.6%) compared with those who didn't get an MRI (89.1%). Yoen said this was mainly due to improved local-regional recurrence rates. However, MRI was not significantly associated with improved overall survival (p = 0.875).
Delving further into the data, the researchers also found a significant association for MRI for decreasing the risk of total recurrence in patients specifically with hormone receptor-negative breast cancer (HR, 0.2; p < 0.01). However, they did not find a significant benefit for patients with hormone receptor-positive cancers (HR, 1.3; p = 0.64).
Yoen said the preoperative breast MRI strategy could be especially helpful for women with hormone receptor-negative cancers as departments try to improve upon breast MRI guidelines.