Most interval cancers are detected via supplemental screening, and most women diagnosed with interval disease have high lifetime risk scores, according to research presented on May 6 at the Society of Breast Imaging (SBI) annual meeting in National Harbor, MD.
The study results highlight the importance of supplemental screening among women at high risk for breast cancer, said presenter Dr. Tiffany Clausen from Florida International University in Miami.
"Supplemental screening is really important, and we can't forget that women with dense breasts or women at higher risk still need this screening, even though we have new technology coming out as a primary screening mechanism," Clausen told AuntMinnie.com.
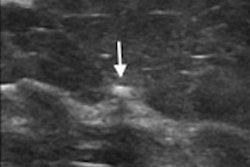
Even as screening breast imaging technology advances, interval breast cancers persist as a challenge. This especially goes for high-risk women, such as those with dense breast tissue. Supplemental imaging such as ultrasound or MRI is used to make up for mammography's limitations in this area.
Clausen's team sought to evaluate the clinical risk assessment, method of detection, and tumor characteristics of women diagnosed with an interval breast cancer after a negative 3D screening mammogram. They included data collected between 2013 and 2022 from 44 women and 158,671 3D screening mammograms, for an interval cancer rate of 0.3 per 1,000 screening exams.
The team reported that out of the 44 cases, 32 were detected by screening breast ultrasound, seven by screening breast MRI, and five by presentation of a palpable lump. Twenty-nine of the women had a Tyrer-Cuzick lifetime score that would be deemed intermediate or high-risk; 37 of the women (84%) had either heterogeneously or extremely dense breast tissue.
The researchers also found that 37 of the women (84%) were diagnosed with invasive carcinoma, 34 being invasive ductal cases and three being invasive lobular cases. The remaining seven women were diagnosed with ductal carcinoma in situ (DCIS).
Overall average invasive tumor size was 1.3 cm, and all but one of the tumors were node-negative. All DCIS cases were hormone receptor-positive. Of the invasive tumors, molecular subtypes included 30 luminal A (81%), four luminal B (11%), one HER2-enriched (3%), and two triple negative (5%).
The results highlight the importance of offering multiple forms of supplemental breast cancer screening to reduce the possibility of a false-negative on 3D mammography, Clausen said, adding that a larger sample size and having a control group to which to compare results would help validate the team's findings.