No matter how safe a radiation oncology department considers its operational procedures to be, more ways can be found to prevent errors from occurring. That's the underlying message of an article published in the July issue of the Joint Commission Journal on Quality and Patient Safety.
Following an in-depth evaluation, researchers at Johns Hopkins' Sidney Kimmel Comprehensive Cancer Center found that its robust quality assurance program and checklist-conscious culture wasn't enough; radiation oncology departments need to regularly and proactively question the safety of everything that's being done.
Lead author Dr. Stephanie Terezakis, an assistant professor of radiation oncology at the Johns Hopkins School of Medicine, and colleagues conducted a failure mode and effects analysis and implemented a voluntary intradepartmental error and near-miss reporting system. They used data from both efforts to prioritize risks and implement risk-reduction strategies (Jt Comm J Qual Patient Saf, July 2011, Vol. 37:7, pp. 291-299).
The authors and their department colleagues identified 269 steps from start to finish in the process of planning and administering radiation therapy treatments. They calculated that if each step were error-proof at the 99.9% level, the cumulative total probability of an error would be approximately 25%. In a prior recent analysis, the department determined that it had a 0.2% error rate.
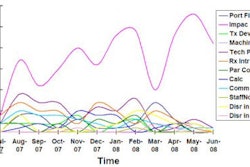
Seeking to improve upon this record, a 14-person committee consisting of representatives from each section of the radiation oncology department was selected. The staff mix included administrators, dosimetrists, nurses, physicians, physicists, and radiation therapists. They created a visual process map, categorizing each of the 269 steps into consulting, simulation, treatment planning, and treatment delivery processes. Two analyses were conducted, one in 2006-2007 and another in 2009.
The committee members identified 127 different possible failure modes in the first analysis and 159 in the second. They assigned each failure mode a risk probability number based on severity, frequency, and ability to be detected. Mitigation strategies were then developed and prioritized. The rankings were particularly useful in terms of providing a structure to prioritize safety improvements, according to the authors.
Seventy-nine possible solutions were identified for the 15 highest ranked failure modes, and 33 solutions were considered as targets for implementation. The committee then developed action plans to immediately implement the chosen solutions.
The following were the top five potential failure modes:
- Incorrectly exporting diagnostic images to record and verify the system
- Needing to re-mark a patient after treatment shifts are made
- Selection of incorrect beams and energy
- Inability to verify that a patient's marks are valid for treatment
- Incorrect treatment plan generated as a result of incorrect contouring by a physician
Error reporting system
The department also implemented a Web-based incident reporting system in July 2007 to gather information about any event that deviated from expectation. Although the system was voluntary, all members of the department were encouraged to use it. To determine if the failure modes identified matched actual incidents, the authors analyzed incidents reported during a three-month period in 2009.
Although the database probably was not inclusive because most entries were submitted by radiation therapists and none were from physicians, 42% of actual errors had not been identified by the failure modes and effects analysis, the group determined. As a result, the department learned that not all potential errors could be identified by the system, even though efforts were undertaken to do so by staff representing all aspects of the treatment process.
Some of the entries in the incident reporting system occurred as a result of communication between caregivers, especially at key handoff points in a patient's care. The department added electronic checklists, which have been incorporated into the electronic workflow. If any near-miss or error is identified, the electronic system forces its appropriate reporting.
"Quality control measures can uncover certain specific errors, such as machine dose miscalibration or misalignments of the patient in the radiation treatment beam," the authors observed. "However, they are less effective at uncovering less common errors that can occur anywhere along the treatment planning and delivery process, even when the process is functioning."
The basic science of radiation treatment has received considerable support and attention in developing novel therapies to benefit patients, concluded Terezakis and colleagues.
"The time has come to apply the same focus and resources to ensuring that patients safely receive the maximal benefits possible," they wrote.