With a reported complication rate of 22%, performing laparotomy in patients who have penetrating stab wounds, but no visceral involvement, is a risky business. These patients would be better served by monitoring with serial ultrasound and contrast-enhanced CT, according to Colombian researchers.
Dr. Jorge Soto and colleagues from the Hospital Universitario San Vicente de Paúl in Medellín evaluated the usefulness of these two modalities for the initial assessment of penetrating abdominal stab wounds. They reported their results in the August issue of Radiology.
"We used both modalities to capitalize on the relative advantages of each: the high sensitivity of CT for the detection of fluid and visceral lesions and the possibility of repeating US examinations for monitoring the amount of free fluid," they wrote (Radiology, August 2001, Vol.220: 2, pp. 365-371).
The prospective evaluation took place over 36 months from April 1997 to March 2000. Out of 202 patients admitted to the emergency department during this time period, 32 met the study criteria and did not require an immediate laparotomy. The majority of the penetrating wounds were in the right upper quadrant (18 patients), with the remainder in the left upper and left lower quandrants.
Within an hour of admission to the ER, all 32 patients underwent real-time ultrasound of the abdomen with a Sonoline S145D using a 3.5-MHz convex transducer (Siemens Medical Systems, Iselin, NJ). The ultrasound exam was repeated 12 hours later with the same equipment and technique, the study stated. The radiologist examined the abdomen for free fluid, and solid organs were checked out for lacerations.
"We calculated the free-fluid index at 12 hours and compared it with that of the baseline study...we considered an increase in the free-fluid index significant if it exceeded 5 cm," they said.
One hour after ultrasonography, all patients underwent helical CT of the abdomen and pelvis with a ProSpeed SX scanner (GE Medical Systems, Waukesha, WI). Two different kinds of contrast agents were administered orally and rectally (800 mL and 500 mL, respectively, of Gastroview, Mallinckrodt, St. Louis), and intravenously (100 mL of Iopamiron, Schering AG, Berlin). CT scan acquisition parameters were 10-mm collimation, 1:1 to 1.5:1 pitch, 28-36-second exposure at one tube rotation, 120 kVp, and 200 mAs.
Soto told AuntMinnie.com that the total examination time for the ultrasound exam was 5 to 7 minutes, and 15 minutes for the CT scan. Interpretation took an additional 5 minutes in each modality.
The reviewing radiologist noted a number of factors as evidence of bowel perforation, including the presence and location of free peritoneal fluid and air and localized mesenteric or peritoneal hematoma.
According to the results, the ultrasound exam demonstrated abnormalities in 43.8% of the patients. Of these 14 cases, 8 had free fluid at admission; the initial sonogram revealed an associated solid organ injury. In one instance, initial ultrasound did not detect a hepatic lesion, but the patient recovered with conservative treatment.
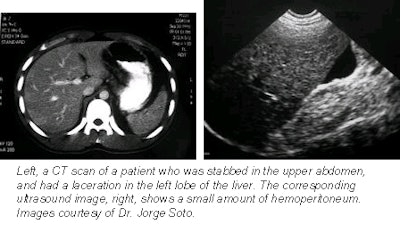 |
In the case of CT, the scan depicted intraperitoneal abnormalities in 65.6% of patients, including free peritoneal fluid and renal laceration. In 12 out of 21 patients, CT showed abnormalities that were not detected with ultrasound, the group reported.
Only one patient required laparotomy after the baseline ultrasound and the CT exam. Despite appropriate fluid replacement, the patient showed signs of peritoneal irritation. An extensive hepatic laceration and hemoperitoneum was found at laparotomy, the authors said.
In general, the group found that CT was more adept at demonstrating hepatic and renal injuries, while US was better for detecting increases in free fluid.
"We prefer [US] because of its lesser cost, lack of ionizing radiation, and greater availability," they said. "The results of our study suggest that [by using the imaging algorithm], the length of hospital stay for many patients may be decreased." Soto told AuntMinnie.com that they have had good results implementing US and CT imaging techniques into their protocol, cutting down on long hospital stays and decreasing morbidity that can result from unrecognized bowel injuries.
Research out of Belgium has come to a similar conclusion, going so far as to suggest eliminating exploratory laparotomy altogether. In a study published in European Journal of Emergency Medicine, investigators from the University of Antwerp wrote: "Routine laparotomy for penetrating trauma to the abdomen proves to be no longer warranted. Clinical and especially diagnostic studies should be able to select patients in whom laparotomy should be performed" (June 2001, Vol.8:2, pp. 83-88).
Another study conducted at North Shore University Hospital in Manhasset, NY, recommended relying on focused abdominal sonography for trauma (FAST) to "accurately determine which patients required operative intervention first, despite that patient's appearance of relative hemodynamic stability in comparison to the other stabbing victim" (Journal of Emergency Medicine, July 2001, Vol.21:1, pp. 41-44).
By Shalmali PalAuntMinnie.com staff writer
August 29, 2001
Copyright © 2001 AuntMinnie.com



















