The technology for breast cancer detection has certainly made great strides in the last 200 years, but the clinical breast exam (CBE) has remained the same since 19th-century surgical pioneer William Halsted performed the first radical mastectomy. Adding a technique called palpation imaging (PI) to CBE may be just the ticket to bring this most basic breast exam into the 21st century.
"A need exists for a device that accurately and objectively depicts the CBE in digital format which is reproducible over time, and able to upload into various electronic medical records," wrote Dr. Cary Kaufman and colleagues in the American Journal of Surgery (October 2006, Vol. 192:4, pp. 444-449).
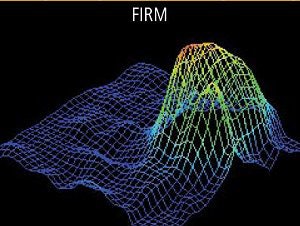
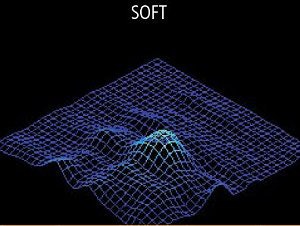
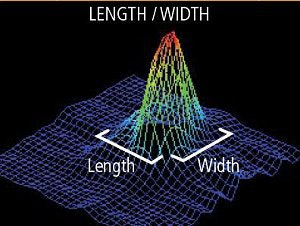
PI captures the characteristics of palpable CBE findings such as estimated size, shape, firmness of breast tissue, and homogeneity of the mass, explained Kaufman and colleagues, who are from the University of Washington and the Bellingham Breast Center, both in Bellingham, WA.
For this two-year study, 110 patients underwent CBE, ultrasound and/or mammography, and assessment with PI (SureTouch Visual Mapping System, Medical Tactile, Los Angeles). As with ultrasound, PI uses a handheld transducer that records the pressure and location of a palpable mass. The data is converted to 2D and 3D color images. The exam video, as well as still frames, can be incorporated into a report or consultation letter.
Based on PI findings only, the patients were divided into two groups: those with a dominant mass (cyst, tumors) and those without a dominant mass (fibrocystic changes). Preoperative PI data was correlated with final histology or at least six months of follow-up information.
According to the diagnostic results, 95 of 110 patients were found to have lesions. PI identified dominant masses in 89 of the 95 patients for a positive predictive value (PPV) of 94%. PI's sensitivity and specificity both came in at 88%. In comparison, physical exam alone turned in a PPV of 86% and 81% sensitivity and specificity.
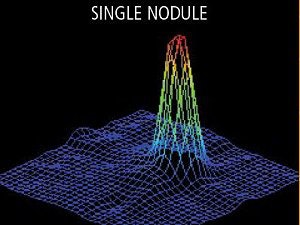
For identifying breast cancer as a mass, the PPV for PI was 94% in 36 cancers versus 78% for physical exam. For fibroadenomas or cysts, 91% of the lesions showed the classic PI findings of a single smooth peak with a firm central mass, the authors stated. Additionally, they noted good correlation between PI findings and ultrasound measurements in these patients.
The study also consisted of a physician survey in which three surgeons wrote up different consultation forms: a longhand report with hand drawings, a typed letter without any drawings, and a typed letter with a printed digital image as well as a report of the PI results. Fifteen referral physicians then rated each surgeon's report.
 |
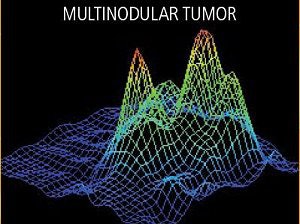 |
| PI captures such lesion characteristics as shape (above), degree of firmness (below), and size (bottom). The peak height of the image refers to increased firmness. The low height refers to less firm or soft tissues. Images courtesy of Medical Tactile. |
 |
 |
 |
Most of the referral physicians favored the typed report with the PI report, ranking that surgeon as the most experienced and as the best communicator. In addition, patients who expressed an interest in their CBE results were able to understand the PI report, the study group added.
The authors pointed out some of the advantages of PI: the device is less expensive than a portable ultrasound unit and can be operated by a surgeon trained in ultrasonography. Most important, PI results can make it easier for a series of specialists to follow a patient's palpable findings.
However, a major strike against PI is that is not currently reimbursed by insurance, Kaufman's group stated. It also requires training and skill to obtain accurate images. Finally, PI should not be considered an alternative to more invasive procedures.
"At no time was PI considered a substitute for biopsy, and biopsy should always be considered as the definitive test for the presence of breast cancer," the group cautioned. Instead, they stressed that PI can boost "chart documentation, communication with other physicians, education for patients, and as a medical record for insurers or medicolegal purposes."
In an e-mail interview with AuntMinnie.com, Kaufman offered more details on PI and how it could impact breast imaging.
AuntMinnie: Could you explain how PI fits into the overall breast exam protocol, starting with CBE by a primary care physician, through imaging, and any potential surgical follow-up?
Kaufman: This device is an objective record of the physical exam. It can be used by any trained clinician, not only a surgeon. In the American Journal of Surgery paper, it was used by surgeons in a consecutive series of women with palpable breast concerns. These women were identified as having a palpable mass by either the referring clinician or by the patient. In this paper we examined each patient as well as reviewing the other examination methods (most had mammograms and ultrasounds as well).
Our protocol was to examine each patient with palpation imaging to both create an objective record of the exam, as well as to compare the palpation imaging with a surgeon's clinical breast examination. Similar to creating other imaging documentation, the PI record becomes part of the patient chart. It objectively documents the patient's physical examination, converting subjective descriptions of "firm" or "glandular" into a permanent visual digital document.
If the surgeon wishes, a copy of the visual digital document may be included with their consultation note, similar to images being delivered along with an x-ray report. This is only one advantage of a digital record, but is timely in view of the increased use of the electronic medical record.
Since this device is primarily a documentation device (at this time) further workup of the palpable findings would occur after the PI examination. This may include needle biopsy or further imaging workup.
On that same topic, could PI results be used to guide additional imaging workup, such whether the patient would benefit from ultrasound or MRI?
At this time, it is being used as a documentation device. It currently does not indicate nor preclude further workup. In the future, algorithms may be developed to improve the diagnostic value of palpation imaging.
Does breast density influence the accuracy of the PI exam?
Breast density requires definition. Breast density as seen by mammography does not seem to influence the accuracy of the PI exam. Breast density as defined by palpation thickness or firmness appears to minimally influence palpation imaging.
For example, women with fibrocystic change may be difficult to examine by palpation. However, using palpation imaging, any underlying true mass such as a benign or malignant tumor is often demonstrated. The 200-plus tactile sensors on the PI examination probe are very sensitive to firmness and can distinguish between dense breast tissue and solid mass.
(Breast density) was not the subject of this publication nor was this discussed in our paper, but we hope to demonstrate these findings in future studies.
You mention in the paper that PI is an operator-dependent device. Do you have information on the learning curve associated with obtaining optimal PI results?
Because of the consistency of the sensors and calibration of the device, (PI) is an examination technique that is readily mastered. The learning curve has not been defined and varies with the clinician's experience with breast examination and breast pathology. Due to the experience that breast surgeons possess, we used surgeons for this publication. Other clinicians may also be candidates for use of this device.
Your group also states that PI results "can be used for ... medicolegal purposes." Given that malignant neoplasm of the female breast is the most prevalent condition resulting in malpractice claims -- and that radiologists are most often sued -- what kind of added "protection" would the PI record offer?
Palpation imaging is an objective device. Regardless of who is using the transducer probe, a trained examiner will obtain the same documented examination on the same patient on the same day. This allows for the creation of an objective record of any palpable findings in the area examined on that particular date.
If there were to be any medicolegal inquiry at a later time as to whether a mass was present or not on that date of examination, the palpation imaging record can be an impartial observer of the actual clinical examination. It would lend credibility to the clinician that, indeed, the clinical findings as described by the clinician and recorded by palpation imaging were accurate and correct. It might be more difficult for a patient to claim that there was a palpable mass present at a time when both clinical examination and palpation imaging documents the lack of a palpable mass.
By Shalmali Pal
AuntMinnie.com staff writer
October 9, 2006
Related Reading
How the legal system stacks the deck against mammography, April 3, 2006
New report slams breast imaging as flawed compared to biopsy, February 9, 2006
Doctors skip breast exam before mammo referral, April 24, 2002
Copyright © 2006 AuntMinnie.com