NEW YORK CITY - The sensitivity of shear-wave breast elastography can be significantly improved by a quality measure that grades the adequacy of the shear wave itself, according to research presented at the American Institute of Ultrasound in Medicine (AIUM) annual meeting.
By incorporating a quality measure that determines whether the shear wave is sufficient in quality to yield accurate measurements, shear-wave imaging sensitivity increased from 41% to as high as 93%, according to Dr. Richard Barr, PhD, of Northeastern Ohio Medical University and Radiology Consultants in Youngstown, OH. These gains came at the cost of a nearly 17% increase in exams that couldn't be evaluated, however, Barr said.
He presented the findings during a Monday scientific session.
There are two types of elastography: strain and shear-wave imaging. Strain, or elasticity imaging (EI), is based on tissue deformation from an external or patient source and is a qualitative study. A quantitative exam, shear-wave elastography applies a "push pulse" that results in shear-wave propagation that can be measured as velocity, Barr said.
"Both strain and shear-wave imaging have been shown to improve characterization of breast masses," he said.
On strain elastography, malignant breast lesions appear larger and benign lesions appear smaller. The ratio of a length of lesion on elastography divided by lesion length on B-mode imaging can be used to characterize lesions as benign or malignant with high sensitivity and specificity, Barr said.
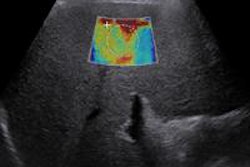
On shear-wave imaging, the shear-wave speed is measured on conventional B-mode images. The shear-wave velocity, Vs, is proportional to the stiffness of the tissue. The harder the lesion, the faster the Vs, he said. Vs can also be measured in a very small voxel, or point of measurement.
Some issues have been reported from shear-wave elastography, however. Some malignant lesions have not been color-coded at all on studies, and some have been coded as blue, or "soft cancer," inappropriately, Barr said.
"In our experience, approximately 50% of invasive ductal cancers either code as 'soft' or have no signal with shear-wave imaging, even if we include the 'ring' of high tissue that is often seen in some of these tissues," he said.
This problem is also not vendor-specific, having been identified on equipment from two vendors on the same case, he said.
Quality measure
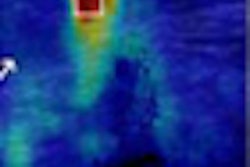
In an attempt to deal with this challenge, the researchers studied the use of a quality map, which grades the shear waves themselves for their quality. The quality of the shear waves are presented in a color-coded map, with different colors used for various quality ratings.
The researchers studied the technique on 144 patients with 166 lesions who were scheduled for ultrasound-guided biopsy. Standard B-mode and color Doppler evaluation was performed, and strain imaging was acquired using a 14 MHz probe on an Acuson S2000 ultrasound scanner (Siemens Healthcare).
Shear-wave imaging was obtained using Virtual Touch Imaging Quantification (VTIQ) mode at 9 MHz on a modified S2000 system. The data was displayed as velocity map and a quality map. For strain imaging, the EI/B-mode ratio was calculated; a ratio less than 1 was considered to be a benign lesion, while a ratio of 1 or greater was considered to be malignant.
On shear-wave imaging, the highest Vs in the lesion or surrounding "ring" was documented. A note was made if there was a "ring" and the quality measurement of the ring and the central tumor was recorded. A Vs less than 4.5 m/sec was considered to be benign, while a Vs greater than 4.5 m/sec was determined to be malignant.
The 144 patients in the study had an average patient age of 48.5 (range 18-81) with an average lesion size of 10.6 mm (range 5-43 mm). The researchers correlated elastography results with pathology and obtained receiver operating characteristic (ROC) curves to assess performance.
There were 110 benign lesions and 56 malignant lesions.
| Elastography performance | ||||
| Evaluable cases | Sensitivity | Specificity | Area under the ROC curve | |
| Strain imaging | 163 | 95% | 88% | 0.9595 |
| Shear-wave imaging without quality measure | 166 | 41% | 95% | 0.6756 |
| Shear-wave imaging with quality measure | 138 | 78% | 94% | 0.7988 |
| Shear-wave imaging with a low-quality measure and a solid lesion | 166 | 93% | 87% | 0.9006 |
Of the benign lesions, 16 (14.6%) had no shear-wave imaging signal, 89 (81%) were benign on shear-wave imaging, and five (4.5%) were judged malignant.
In the malignant lesions, shear-wave imaging had no Vs results in 10 lesions. Twenty-five (44.6%) were considered benign and 31 (37.5%) were judged malignant.
The researchers found that the quality measure was low in all cases where no shear-wave imaging signal was obtained. It was also low in 19 (76%) of 25 soft malignant lesions and in two (40%) of five hard benign lesions. In soft benign lesions, the quality measure was low in only six (6.7%) of 89 cases.
In other findings, the researchers noted that the quality measure was high in three (12%) of 25 soft malignant lesions, which were lymphomas. Three false negatives on elasticity imaging were lymphomas, according to the researchers.
In cases where there is a low quality measure, if the lesion is solid, it is most likely a cancer, Barr said.
Both strain and shear-wave elastography provide additional information on breast lesion characterization, he concluded.
"Strain had the highest sensitivity, but shear wave had the highest specificity," Barr said. "The combination of [elasticity imaging] and [shear-wave imaging] may increase confidence and accuracy in characterizing breast masses."