Ultrasound may be the imaging modality of choice for surveillance of hepatocellular carcinoma (HCC) in high-risk patients, but variance in exam quality can be a big problem, according to researchers from the University of California, San Diego (UCSD).
In a small, retrospective review, the UCSD team found that nearly two-thirds of ultrasound studies performed for HCC surveillance were considered inadequate in quality, as determined by visualization and penetration of the liver. Key factors affecting exam quality included high body mass index (BMI), ascites, and the presence of cirrhosis, according to Dr. Yuko Kono, PhD, an associate clinical professor of medicine in the division of gastroenterology and hepatology and an associate clinical professor of radiology.
She presented the group's findings during a scientific session at the annual American Institute of Ultrasound in Medicine (AIUM) meeting in Orlando, FL.
Varying sensitivity
While all major liver societies recommend ultrasound for surveillance of HCC in high-risk patients, the modality's sensitivity for detecting early HCC during surveillance can vary significantly, according to Kono. Prior research has found sensitivity levels ranging from 23% to 98%, with a pooled sensitivity of 69%.
However, to date, no studies on HCC surveillance have assessed the quality of ultrasound and the factors that affect it, or linked ultrasound quality with efficacy, she said.
As a result, the researchers set out to investigate the quality of ultrasound in the context of HCC surveillance and to elucidate its contributing factors. They performed a retrospective review of all ultrasound studies conducted at their institution in 2012 for HCC surveillance. Of the 194 studies ordered during this period, 80 were excluded because the patients had known HCC or the ultrasound was performed for other purposes.
The researchers analyzed a number of factors, including patient demographics and laboratory values, for the remaining 114 patients, 99 of whom were cirrhotic and 15 of whom had hepatitis B without cirrhosis.
They also reviewed the ultrasound reports and charts to determine whether the liver lesions were detected and subsequently diagnosed as HCC. Next, an experienced radiologist rated the quality of the ultrasound studies based on the visual clarity of the liver, penetration, and noted exam limitations. The studies were categorized as follows:
- Excellent: Complete visualization of the entire liver and full penetration
- Good: Complete visualization of the liver but limited penetration
- Fair: Parts of the liver could not be clearly visualized as penetration was inadequate
- Poor: Visualization and/or penetration were significantly limited
Six months later, the same radiologist repeated the image-quality assessment to assess intrarater reliability.
| Quality ratings for HCC ultrasound | |||
| Rating | 1st quality assessment | 2nd quality assessment | Average |
| Excellent | 9.9% | 6.3% | 8.1% |
| Good | 27.9% | 30.6% | 29.3% |
| Fair | 24.3% | 21.6% | 23% |
| Poor | 37.8% | 41.4% | 39.6% |
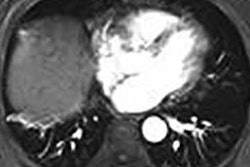
 Examples of poor-quality (above) and good-quality (below) images. All images courtesy of Dr. Yuko Kono, PhD.
Examples of poor-quality (above) and good-quality (below) images. All images courtesy of Dr. Yuko Kono, PhD.Many inadequate studies
An average of 37.4% of the studies were considered adequate (rated as excellent or good), while an average of 62.6% were judged to be inadequate (rated as fair or poor), the researchers found.
A high BMI (p ≤ 0.001), ascites (p = 0.039), and cirrhosis (p = 0.042) were considered the main limiting factors in the quality of the inadequate studies, according to multivariate analysis. Liver international normalized ratio (INR) was not a statistically significant factor (p = 0.089).
Nine cases of liver lesions were identified using ultrasound, but none were HCC.
"To date, no HCC cases have been found in this cohort," Kono said.
Intrarater reliability showed substantial agreement (kappa = 0.0748) for the image quality ratings.
"Of course, more studies are needed on a larger scale to assess ultrasound quality, its contributing factors, and its influence on the effectiveness of HCC surveillance," Kono said.
Disappointing results
In a comment after the presentation, Dr. Stephanie Wilson, of the University of Calgary, noted that the study results were disappointing.
"One of things I've always thought is such a tragedy was that ultrasound surveillance was implemented without good documented evidence that it was a good thing to do," Wilson said. "I feel ultrasound does do a great job as a surveillance tool, and I think it would be such a great thing for ultrasound if we could somehow have better evidence that it is a good screening modality."
Kono agreed, in particular because HCC surveillance is currently being performed on only a fraction of the high-risk patients in the U.S. for whom it's recommended.
"And without ultrasound, how can we [increase utilization of surveillance]?" she asked. "We need to do [the ultrasound] properly and we need to document it properly, and then we need to [understand] the implications when it's not a good quality and we need other modalities to help."
A large study found that only 18.4% of high-risk patients diagnosed with HCC had received CT or ultrasound imaging surveillance for HCC in the year before diagnosis.
"It's very shocking, and we need to really educate more primary care doctors, gastroenterologists, and patients and have more surveillance," Kono said.