The long-term effects of COVID-19 were evident on images acquired with point-of-care ultrasound scanners (POCUS) used to monitor the recovery of patients who experienced severe cases of the disease. Researchers described their findings in a November 13 article in the Journal of Ultrasound in Medicine.
The international research team documented pulmonary abnormalities in almost half of patients four months after discharge from intensive care unit (ICU) admission. The findings support point-of-care ultrasound (POCUS) as a promising radiation-free imaging modality for long-term patient follow-up.
"POCUS showed ability to monitor the evolution of severe COVID-19 pneumonia after hospital discharge, supporting its integration in clinical predictive models of residual lung injury," wrote the authors, led by Dr. Abdulrahman Alharthy, head of the ICU at King Saudi Medical Center in Riyadh, Saudi Arabia.
The prospective study included 171 patients with laboratory-confirmed cases of COVID-19 who required ICU treatment in April. All patients experienced severe COVID-19 with acute respiratory failure.
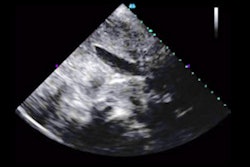
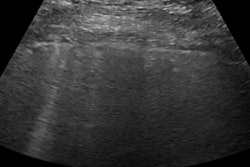
On ICU admission, POCUS revealed hallmark COVID-19 findings, including B-lines, irregular pleural lines, and consolidations. Abnormalities were more common in the right lung than the left.
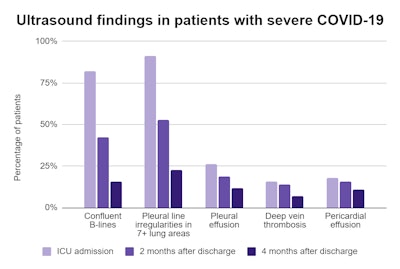
Out of the 171 study participants, 127 survived their hospital stay and participated in two- and four-month follow-up ultrasound scans. The scans showed many patients still had B-line-like artifacts and pleural line irregularities; however, the incidence of abnormalities detected by POCUS significantly decreased over time.
Notably, nearly half (49%) of the survivors remained symptomatic, defined as having difficulty breathing, experiencing fatigue, and being unable to complete a six-minute walk test. The sheer number of patients with lingering symptoms four months after discharge surprised the research team.
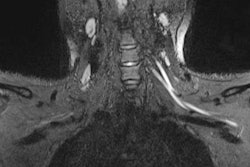
Patients with lingering symptoms had significantly more lung abnormalities detected after discharge than asymptomatic patients. While the majority had no apparent lung conditions, 15 patients developed interstitial lung disease confirmed by chest CT scans that showed peripherally distributed ground-glass opacities with lower lobe predilection.
"The follow-up period turned out to be too short to fully elucidate the clinical course of the newly diagnosed [nonspecific interstitial pneumonia] in these patients," the authors wrote.
The findings come on the heels of another Journal of Ultrasound in Medicine study documenting lung abnormalities in patients who had recovered from mild cases of COVID-19. Both research articles highlight the long-term implications of COVID-19 as well as the importance of follow-up imaging to monitor patients for additional complications.
"The ability of POCUS in detecting the evolution of COVID-19 pneumonia justifies its utilization in clinical models that could be used to predict the severity and outcome of multifaceted crucial illness as well as the residual lung injury post-hospital discharge," the authors wrote. "This study provides further insight about the long-term sequelae of COVID-19 pneumonia and outlines the need for monitoring of survivors."