Ultrasound has higher sensitivity but also higher false-positive rates than clinical examination alone when it comes to detecting skin cancer in the head and neck areas that may have spread to the lymph nodes.
A team led by Selin Tokez from the University Medical Center Rotterdam in the Netherlands found that while relying on clinical examination alone can miss cancers, adding ultrasound can lead to unnecessary procedures.
"Ultrasonography had high sensitivity for detecting nodal metastases, but this sensitivity should be evaluated against the high rate of false-positive findings," Tokez and colleagues wrote in research published December 29 in JAMA Dermatology.
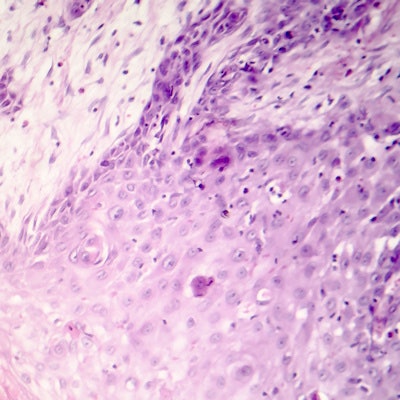
Cutaneous squamous cell carcinoma is the second most common type of skin cancer among white patients. While these carcinomas are generally curable with a low mortality risk, the risk of metastasis is between 1.5% and 5.2%, the researchers said.
Additional workup is usually performed if lymph node metastasis is suspected during clinical examination. However, there is no standard for what type of routine lymph node screening is needed for patients with cutaneous squamous cell carcinoma.
Ultrasound is commonly requested for suspicious clinical examination cases, but little is known about whether it adds value when no palpable lymph nodes are present.
Tokez et al wanted to find out the diagnostic accuracy of clinical examination and baseline ultrasound for finding lymph node metastasis in patients with high-risk squamous cell carcinoma of the head and neck area. They also wanted to find out how accurate the modality is in finding occult metastatic disease among patients with a negative result at baseline clinical examination.
They looked at data from 233 patients with a total of 246 high-risk tumors of the head and neck area. The researchers found that out of 22 cytologically confirmed metastases, ultrasound correctly detected 20 metastases compared with the 11 correctly identified by clinical examination alone.
| Ultrasound vs. clinical exam in detecting lymph node metastasis in squamous cell carcinoma | ||
| Clinical exam | Ultrasound | |
| Sensitivity | 50% | 91% |
| Specificity | 96% | 78% |
| Positive predictive value | 55% | 29% |
| Negative predictive value | 95% | 99% |
Ultrasound also detected nine of 11 metastases in the group of 226 patients with negative results at clinical examination. Here, it showed a sensitivity of 82%, a specificity of 79%, a positive predictive value of 17%, and a negative predictive value of 99%.
The researchers said one possible explanation for ultrasound's low positive predictive value was the low threshold used in their tertiary center to consider a lymph node suspicious, leading to the need for fine-needle aspiration cytology. This means a relatively high number of negative results after cytology procedures.
The study authors also said there is a lack of data on prognostic outcomes after radiologic imaging of these tumors.
"Future studies are needed to identify the specific populations with cutaneous squamous cell carcinoma who would most benefit from the addition of baseline ultrasonographic evaluation to detect occult metastatic disease," they added.
In an accompanying editorial, Dr. Emily Ruiz from Brigham and Women's Hospital in Boston said added healthcare expenditures and burdening elderly patients with more medical visits should be considered before implementing imaging.
"To my knowledge, there are no studies of the cost-effectiveness of radiologic staging and surveillance in cutaneous squamous cell carcinoma," Ruiz wrote. "However, because ultrasonography is inexpensive and can be combined with a routine clinic appointment when performed by the treating physician, it may be more cost-effective than other modalities."




















