General radiologists who undergo training in the BI-RADS lexicon showed a marked improvement in their ability to classify lesions, as well as make biopsy recommendations. Furthermore, BI-RADS-trained radiologists are more likely to retain and recall the material months later.
Dr. Wendie Berg, Ph.D., and colleagues discussed their experience with a custom-designed BI-RADS lexicon one-day course that was used to train 27 radiologists in September 1999. Berg is from the department of radiology and the Greenebaum Cancer Center at the University of Maryland in Baltimore.
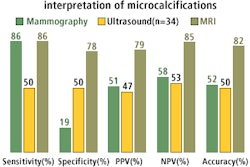
"A set of 54 ‘quiz’ cases was developed (by Berg) from prospectively nonpalpable lesions representative of the BI-RADS lexicon for mass margins and microcalcification morphology and distribution," the authors explained (Radiology, September 2002, Vol. 224:3, pp. 871-880).
These lesions were selected as pure examples of individual features of the BI-RADS lexicon. Photographic slides were prepared that centered on the area of interest. The final assessment ranged from category 2 (benign) to category 5 (highly suggestive of malignancy).
During the course, the researchers showed slides of the quiz cases, followed by a question period during which participants were asked to provide a description and a BI-RADS final assessment. The quizzes were shown at the beginning of the day and then again after a lecture on BI-RADS.
Observer performance was measured using k values, with a k value greater than 0.75 indicating excellent agreement; a k value of less than or equal to 0.40 and greater than or equal to 0.75 indicating fair to good agreement; and a k of less than 0.40, poor agreement.
Three experienced breast imagers -- Dr. Carl D’Orsi from the University of Massachusetts in Worcester; Dr. Valerie Jackson from Indiana University in Indianapolis; and Dr. Lawrence Bassett from the University of California, Los Angeles -- also participated in the training.
According to the results, agreement among the expert readers resulted in a generalized k value of 0.57 for mass margins and asymmetries. For the participants prior to training, the generalized k value for all mass descriptors was 0.36. After 1 day of training, the generalized k value improved to 0.41.
For microcalcification morphology, the generalized k value among the experts was 0.44. For the participants, that value increased from 0.36 to 0.44 after the class.
The generalized k value for experienced breast imagers for all microcalcifications was 0.44. Pre-class, the trainees had a generalized k value of 0.35, which increased to 0.36 after the course.
In the final-assessment BI-RADS category, the generalized k value for the breast imagers was 0.51 (category 2); 0.04 (category 3); and 0.50 (category 4-5).
"The overall generalized k value improved (for participants) from 0.31 before training to 0.45 after training," the group reported. With training, 65% of the students showed improved agreement; 22% had no change; and 13% had decreased agreement with the consensus.
The mean biopsy rate for malignant lesions improved, from 73% before training to 88% after training. There was no significant change seen in the biopsy rate for benign lesions after training.
Two to three months later, a subgroup of 11 participants was shown the quiz cases again in random order. Of these 11 readers, 82% retained information with regard to mass and/or asymmetry description. The majority of the participants also maintained the improved k value (0.44) for microcalcification morphology.
However, "less success was maintained for calcification distribution, with four (36%) of the 11 observers showing persistent improved agreement with consensus," Berg and co-authors stated.
For final assessment, 82% of the 11 retained significant improvement.
Overall, identifying calcifications proved more problematic for the course participants than did masses. But the study found that participants were able to maintain their ability to describe suspicious lesion features, such as microlobulated and indistinct mass margins, focal asymmetric densities, and amorphous and pleomorphic calcifications.
A subgroup of participants were able to retain their training 2-3 months after the course, although over time, all participants showed a decrease in k values compared with their immediate post-training scores. This trend suggests that immediate feedback is the source of improvement, the authors stated.
By Shalmali PalAuntMinnie.com staff writer
October 4, 2002
Related Reading
MRI matched with BI-RADS could increase true positive rate for breast biopsy, April 4, 2001
Multiple-reading protocol bolsters interpretation for non-mammographers, September 6, 2002
Reading mammograms: the good, the bad, and the suspicious, July 3, 2002
Mammography reader volume directly linked to diagnostic accuracy, March 6, 2002
Tabár prevails upon mammographers to focus on stellate, not debate, February 27, 2002
Copyright © 2002 AuntMinnie.com