Legislation is advancing in the New Jersey Assembly that would require health insurers to cover additional breast screenings if a mammogram demonstrates dense breast tissue, according to a bill by sponsor Troy Singleton (D-Burlington).
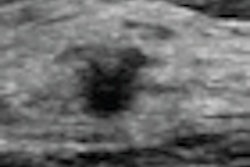
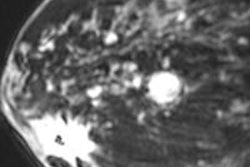
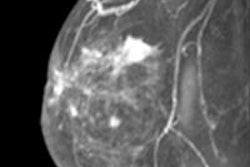
Bill A-2022 would require that, in addition to the existing health benefits coverage requirement for mammograms under state law, health insurers must provide coverage for an ultrasound evaluation, an MRI scan, a 3D digital mammography exam, or other additional testing deemed medically necessary by the patient's healthcare provider after a baseline mammogram shows extremely dense breast tissue.
The provisions of the bill would apply to any group or individual medical service corporation contract providing hospital or medical expense benefits. It is the third such piece of legislation that addresses the issue of insurance coverage of supplementary breast imaging, after Connecticut and Illinois, according to Dr. Nancy Cappello, president of Are You Dense Advocacy.
"A mammogram will detect only about 48% of tumors in women with dense breast tissue, meaning the rest will elude early detection," Singleton said in a statement. "When it comes to our mothers, wives, and daughters, we should be doing everything we can to make sure they have a leg up in the fight against breast cancer."
In addition to Singleton, the measure is sponsored by Assembly Democrats Daniel Benson, Gordon Johnson, Pamela Lampitt, Annette Quijano, and Valerie Vainieri Huttle. It has been approved by New Jersey's Assembly Appropriations Committee and now awaits consideration by the full Assembly.