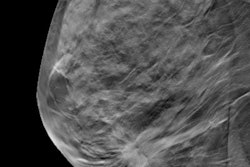
Digital breast tomosynthesis (DBT) is an effective breast cancer screening tool for women of all ages -- including those younger than 50, who may be prone to a higher rate of false positives, according to a presentation given on Sunday at the RSNA annual meeting.
The findings address what some call one of mammography's "harms": high recall rates and false positives, particularly in younger women. Yet DBT has demonstrated lower recall rates and higher cancer detection rates than digital mammography -- benefits that apply even to women ages 40 to 49, who often experience more false positives, said presenter Dr. Liane Philpotts of Yale University.
"Mammographic screening is often criticized due to the balance of false-positive recalls with true cancer detection, and since younger women have lower incidences of breast cancer, the metrics of screening are inherently tipped more toward the harms," Philpotts told session attendees. "But screening DBT's lower recall rates and higher cancer detection rates compared to 2D mammography shift that benefit-to-harm ratio."
Parsing performance
Yale introduced DBT at its main hospital in 2011 and added it to two satellite offices over the next two years, according to Philpotts.
"We offer DBT to all of our patients, free of charge and regardless of their age, risk level, and breast density," she noted.
For the study, Philpotts and colleagues investigated the performance metrics of screening DBT by analyzing 46,140 DBT screening exams taken over a four-year span at the main hospital and the two satellite offices. Women were sorted into five-year age-group intervals, starting at 40 and continuing through 80; the researchers then identified true-positive, false-positive, true-negative, and false-negative cases, and they calculated DBT's overall sensitivity, specificity, and accuracy. The data were also separately analyzed for baseline versus incidence exams.
Philpotts' team found an overall recall rate of 8% (range, 4.9% to 11.6%). The cancer detection rate increased with age (range, 3 cancers/1,000 women screened to 10.6 cancers/1,000 women screened).
Other performance metrics included the following:
- DBT's sensitivity was higher in the 40-to-44 age group (86.4%) than in the 45-to-49 age group (82.8%).
- Overall accuracy for baseline exams decreased with age, with the best accuracy found in the 40-to-44 group (80%) and the lowest in the 70-to-74 group (65%).
- Specificity and accuracy increased as women aged, ranging from 88.7% in the 40-to-44 group to 96% in the oldest groups.
- Incident mammography had higher accuracy than baseline in all age groups except for women 80 and older, while baseline mammography's accuracy decreased with age, with the best accuracy found in the 40-to-44 group.
"When we assessed only the incidence exams, we found no significant difference in screening outcomes between the 40-to-44-year-old group and the 45-to-49-year-old group," Philpotts said. "Although accuracy is slightly lower in younger women, this effect is erased once nonbaseline exams are compared."
What's the takeaway? Screening DBT performs at a high level and with similar accuracy between age groups, such that younger women should not be deterred from undergoing screening, Philpotts concluded.
"Delaying baseline screening until older ages could actually be less effective," she said.
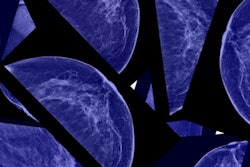
Identifying architectural distortions
In a study presented during the same session, researchers from Brown University shared findings that attest to DBT's effectiveness in a different way: its ability to better identify architectural distortions when compared with mammography -- which can reduce the variability of results between exam readers and increase readers' confidence in their interpretations.
Architectural distortions are a subtle manifestation of breast cancer, and they can be difficult to find, according to presenter Dr. Elizabeth Dibble.
"Architectural distortions are the most commonly missed abnormality on false-negative mammograms and have high interobserver variability," she said. "Minimizing this variability is the best way to reduce inconsistencies in screening mammography interpretation."
For their research, Dibble and colleagues searched for the terms "architectural distortion" or "possible architectural distortion" on screening exams taken at a tertiary breast center between March 2012 and November 2013.
The group recorded patient demographics, imaging and pathology findings, and follow-up imaging results. Two breast radiologists and two breast imaging fellows blinded to exam outcomes reviewed images of two patient groups in four sessions: group A, mammography only, and group B, DBT only; then a month later, group A, DBT only, and group B, mammography only.
Readers recorded whether architectural distortions were present and rated their confidence in their interpretation on a scale of 1 to 4.
The researchers also compared confidence ratings between the two modalities and between attendings and fellows, evaluating interpretation agreement by breast rather than by patient.
Dibble and colleagues identified 59 patients with architectural distortions and 59 control patients. Of the women with architectural distortions, 79.7% had heterogeneously or extremely dense breasts, while 78% of the controls had heterogeneously or extremely dense tissue. Interobserver variability for mammography was 0.53 for right breasts and 0.57 for left; interobserver variability for DBT was 0.72 for right breasts and 0.69 for left. In addition, reader confidence was higher with DBT, reaching statistical significance.
"Reader confidence and sensitivity for detecting architectural distortions was higher for tomosynthesis than for 2D mammography," Dibble said. "We also found that specificity was high with 2D mammography, and remained so with tomosynthesis, which demonstrates that tomosynthesis' increased sensitivity didn't come at a cost to specificity."
DBT decreases interobserver variability, increases reader confidence, and improves sensitivity in the detection of architectural distortions, Dibble concluded.
"Our findings suggest that tomosynthesis may lead to improved detection of this subtle manifestation of breast cancer," she said.