WASHINGTON, DC - While digital breast tomosynthesis (DBT) increases radiation exposure for women when used with digital mammography for screening, the combined dose remains well within safety standards, according to a study presented on Monday at the American Roentgen Ray Society (ARRS) meeting.
The radiation dose delivered to women undergoing DBT in combination with 2D digital mammography varies based on breast density as well as compressed breast thickness. But either way, the dose is well within established guidelines from the U.S. Food and Drug Administration (FDA).
"When DBT is added to standard and digital mammography, the dose is approximately twice the digital mammography dose, but it remains well below the limits set by the FDA," said lead author Dr. Samia Sayegh from NYU Winthrop Hospital in Mineola, NY. "Although there is higher radiation exposure when using DBT with patients with larger or less dense breasts, the risk of this increased radiation requires further investigation."
Breast modalities
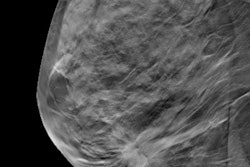
For decades, conventional 2D mammography has played a key role in breast cancer detection. The introduction of full-field digital mammography represented an advance in cancer detection, but its efficacy is sometimes hampered by the inability to discern overlapping structures in the breast.
Then, in 2011, the FDA cleared the first DBT system for breast cancer screening in conjunction with standard and digital mammography. DBT acquires images from an x-ray source positioned over a compressed breast to provide a clear and more accurate view of abnormalities. Previous studies have shown that the technology can increase cancer detection, reduce callback rates by as much as 28%, and bring greater peace of mind to patients and clinicians.
"The combination of DBT plus digital mammography addresses the limitations of conventional mammography by increasing the amount of breast cancers detected and reducing false positives for breast screening in the U.S. and elsewhere," Sayegh told attendees at ARRS 2018. "The major advantage of breast tomosynthesis is decreasing [cancer] detection challenges, especially with overlapping structures in the breast, which is the primary drawback of digital mammography."
While DBT is beneficial for detecting breast cancer, the increase in radiation dose and higher cost of the scan suggest the modality is most helpful in patients with scattered fibroglandular dense tissue and those with heterogeneously dense breasts. In these two patient populations, studies have confirmed DBT's increased detection of cancer, especially for small, invasive cancers, she said.
"But do any of the benefits associated with DBT come with any associated risks?" Sayegh posed. "There is not much literature about additional radiation exposure when DBT is added to 2D mammography with various breast compositions."
Density vs. thickness
For this study, the researchers retrospectively analyzed 203 patients who underwent both digital mammography and DBT to determine the relationship between increased radiation and breast thickness and density. The subjects, who had an average age of 56.2 years, were divided into four groups based on breast density: fatty, scattered fibroglandular, heterogeneously dense, and dense tissue.
The patients' mean breast thickness was 57 (± 16) mm, with the greatest average thickness in the fatty breast group (60 mm) and the least average thickness in the dense breast group (45 mm).
The results were interpreted by two radiology residents and two attending clinicians. The quartet recorded a patient's average radiation dose per view for both DBT and digital mammography, as well as her breast density and thickness.
For the four patient groups, the researchers found a mean total radiation dose of 4.10 (± 1.38) mGy. In separating the two modalities, the mean radiation dose was 1.90 (± 0.73) mGy from digital mammography and 2.2 mGy from DBT.
Additionally, there were no significant differences in total radiation dose across the four groups. Most notably, the mean radiation dose from DBT was significantly greater in the fatty group (p < 0.001) versus the other three patients groups.
| Radiation dose for DBT and 2D mammography based on breast density | ||||
| Type of breast tissue | No. of patients | Mean total radiation dose (mGy) | Mean total radiation dose adjusted for 2D digital mammo (mGy) | Mean radiation dose from DBT (mGy) |
| Fatty | 28 | 4.67 ± 1.13 | 4.57** | 2.7* |
| Scattered fibroglandular | 93 | 4.17 ± 0.92 | 4.20 | 2.2 |
| Heterogeneously dense | 60 | 3.98 ± 1.55 | 3.85*** | 2.1 |
| Dense | 22 | 3.90 ± 1.71 | 3.79*** | 1.9 |
**Significant difference between fatty group and other three groups (p > 0.0001)
***No significant difference between heterogeneously dense and dense groups (p = 0.83)
The researchers also analyzed total radiation dose to patients based on their compressed breast thickness. Interestingly, when adjusted for breast thickness, radiation exposure was significantly greater in the dense breast group (4.79 mGy), followed by the heterogeneously dense group (3.81 mGy), those with scattered fibroglandular tissue 3.81 mGy), and those with fatty tissue (3.53 mGy) (all p < 0.001).
"Unadjusted data showed that fatty breasts receive significantly more radiation than denser breasts, but when we adjusted data for breast thickness, dense breasts saw significantly more radiation than less dense breasts," Sayegh said.
The researchers cited several limitations of the study, such as the small patient sample and the fact that it was conducted at a single center.
"This relationship between breast thickness and breast density is somewhat uncertain, but our study is likely applicable to accept higher radiation doses for thicker [fatty] breasts and denser breasts when adjusted for thickness," Sayegh concluded. "While there is higher radiation exposure with DBT with larger, fatty breasts, this risk of increased radiation requires further investigation."