Digital breast tomosynthesis (DBT) has a lower recall rate compared with full-field digital mammography (FFDM), making it an effective breast cancer screening tool, according to a study published online February 13 in Academic Radiology.
The findings further confirm DBT's value -- particularly when paired with prior mammograms for comparison -- since it reduces false positives and therefore the cost, inconvenience, and psychological stress that can come with them, the researchers wrote.
"Our data show a statistically significant decrease in recall rate with DBT compared to FFDM ... which is also consistent with several prior studies," noted the team, led by Evan Honig of Johns Hopkins University School of Medicine in Baltimore.
Honig's group sought to explore whether any patient and imaging characteristics are associated with false-positive results on screening mammography. To do this, the team conducted a study that included 22,055 screening mammograms acquired between August 2015 and September 2016. Of these, 5,029 (22.8%) were FFDM exams and 17,026 (77.2%) were DBT exams.
The researchers defined false-positive exams as those categorized as BI-RADS 1 or 2 at diagnostic imaging evaluation with one year of cancer-free follow-up, as BI-RADS 3 at diagnostic imaging evaluation with two years of cancer-free follow-up, or those with benign biopsy results.
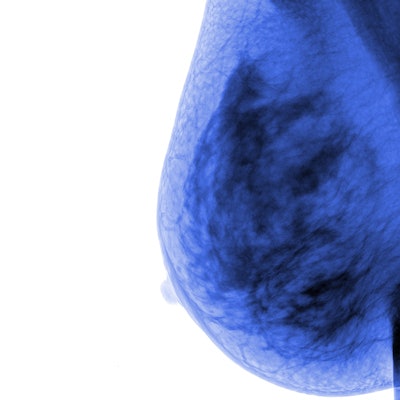
| DBT vs. FFDM by recall rate | ||
| FFDM | DBT | |
| No. performed | 5,029 | 17,026 |
| No. recalled | 531 | 1,356 |
| Recall rate | 10.6%* | 8%* |
Of all the mammograms performed, 1,887 were recalled, for an overall rate of 8.6%. However, by mammogram type, the rates were different: DBT had a rate of 8%, while FFDM had a rate of 10.6% (p < 0.001).
Honig and colleagues also found that false-positive results were lower if prior mammograms were available (90.8% compared with 95.8%, p = 0.02) and if a woman had a previous benign biopsy (87.6% compared with 92.9%, p = 0.01). They did not find statistically significant differences in false-positive results due to factors such as high-risk lesions, family history of breast or ovarian cancer, hormone use, breast density, race, or body mass index.
The study results make clear that DBT should be used as a breast cancer screening tool, and the group hopes that this research will have a positive effect on screening, the authors wrote.
"For future work, we hope to perform similar studies with colleagues who work in a variety of clinical settings," the team concluded. "This will inform us about the potential to scale this work and have a greater impact on the accuracy of screening mammography."