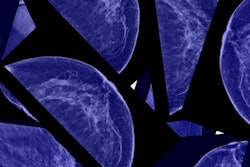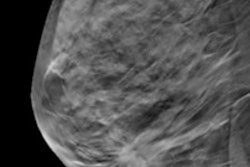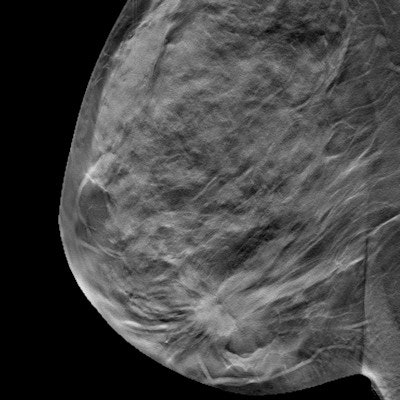
Radiologists who switch from 2D mammography to digital breast tomosynthesis (DBT), or 3D mammography, see improvements in their screening performance that are sustained over time, according to a study published online February 26 in Radiology.
These performance improvements show up for both breast imaging specialists and general radiologists, according to the researchers.
"The average within-radiologist recall rate decreased shortly after DBT adoption both for breast imaging subspecialists ... and for [generalist] readers, without a corresponding decrease in average cancer detection rate," wrote the group led by Diana Miglioretti, PhD, of the University of California, Davis.
The U.S. Food and Drug Administration (FDA) requires only eight hours of training for radiologists to interpret DBT exams. But do radiologists actually need more time? Miglioretti's team explored whether a learning curve was involved in the switch from reading 2D mammography to reading 3D mammography.
The study included data from 106,126 DBT and 221,248 2D mammography exams in 271,362 women. The exams were performed between 2010 and 2017 in 53 facilities in the Breast Cancer Surveillance Consortium (BCSC) and interpreted by 104 radiologists. Miglioretti's group compared the radiologists' screening interpretation performance one year before the adoption of DBT with their performance two years after its implementation.
Switching from 2D to 3D mammography lowered the radiologists' recall rates but didn't affect their cancer detection rates, the researchers found. These results appeared regardless of a woman's breast density.
| Radiologists' recall, cancer detection rates before and after implementation of DBT | ||
| Performance measure | Before DBT (2D mammography) |
After DBT (3D mammography) |
| Mean recall rate | 10.4%* | 9.4%* |
| Mean cancer detection rate | 4 per 1,000 screens | 4.6 per 1,000 screens |
"We found no evidence of a learning curve for the clinical interpretation of screening DBT studies," the team wrote.
Finally, the researchers also discovered that, relative to 2D mammography, the 3D recall rate of the radiologists continued to decrease as the radiologists read more DBT studies.
The fact that both specialized and nonspecialized radiologists improved screening performance is notable, wrote Dr. Regina Hooley of Yale School of Medicine in New Haven, CT, in an accompanying editorial.
"The results of this study are important because the authors showed that the well-established benefits of DBT are present among subspecialist breast imagers and nonspecialist radiologists throughout the United States, and that a significant reduction in screening recall rates can be seen in the immediate DBT adoption period," she noted.