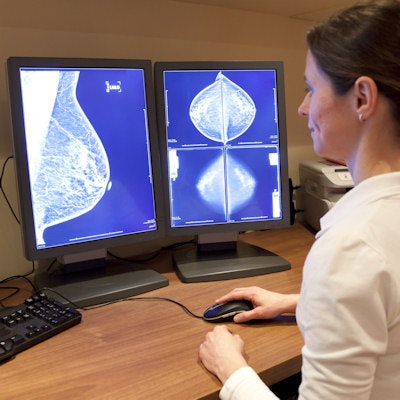
What will it take for artificial intelligence (AI) to become clinically viable in women's imaging? The technology must demonstrate excellence in four crucial areas: performance, time, workflow, and cost, according to an article published online February 19 in the American Journal of Roentgenology.
Key metrics are needed to objectively quantify the potential impact of AI on the practice of radiology, Dr. Ray Mayo and Dr. Jessica Leung of the University of Texas MD Anderson Cancer Center stated in the opinion article.
"As patients, physicians, hospitals, and insurance companies look for value, AI must earn a role in medical imaging," they wrote.
Most importantly, AI must show that it can improve the performance of mammography, the authors noted. Otherwise, the technology won't have utility for interpretation purposes.
Currently available computer-aided detection (CAD) software yields acceptable sensitivity but has a high rate of false-positive marks. These can distract the interpreting radiologist and lead to unnecessary workups and biopsies, according to the authors.
"If AI earns a place in breast imaging, its best opportunity is to decrease false-positive flags compared with the number associated with currently available CAD programs," Mayo and Leung wrote.
Ideally, AI CAD would require no more additional time for radiologist evaluation than currently available CAD software does. AI CAD could also decrease interpretation time by providing fewer flags for radiologists to review, they explained.
"If even a small percentage of cases can be identified as negative with 100% certainty, a substantial amount of valuable physician time can be directed at more complicated cases and other activities requiring human intervention," they wrote.
Of course, AI algorithms must be seamlessly integrated into the workflow.
"The AI effort should start before image acquisition by combing the medical record to identify patients in need of appropriate imaging," they wrote. "The ordering process and scheduling may then be initiated automatically on behalf of the referring physician."
Next, the radiologist's review of the AI image analysis should be completely integrated into the postacquisition process and not require separate workstations or monitors. Furthermore, AI algorithms must be compatible and fully integrated with multiple vendors' hardware and software systems and be functional across varying platforms, according to the authors.
In addition, the cost to provide AI interpretive assistance must not be so high that it tilts the value equation against its use. CAD is currently included as part of a bundled charge for both screening and diagnostic mammograms, and a new billing code is unlikely, they wrote.
"Given that false-positive mammograms are estimated to cost the healthcare system approximately $4 billion each year, a decrease in false-positive CAD flags has strong potential to lower the overall cost of breast imaging," Mayo and Leung noted.
"If developers can achieve the conditions we outline, AI will have an attractive cost-benefit ratio in women's imaging," they concluded.



















