There's enough evidence to support surgical excision of flat epithelial atypia (FEA) breast lesions, according to a meta-analysis published on January 22 in Radiology: Imaging Cancer. These types of benign breast lesions were upgraded to cancer 5% of the time in the new study.
The analysis included dozens of retrospective studies and nearly 2,500 patient cases. The 5% upgrade rate was similar to prior research and above the recommended BI-RADS threshold of 2% for surgical excision of lesions, the authors noted.
"Therefore, our results indicate that FEA diagnosed at core needle biopsy should be managed with surgical excision," wrote the researchers, led by Dr. Rifat Wahab, assistant professor of radiology at the University of Cincinnati Medical Center.
Flat epithelial atypia is a type of benign breast lesion that often presents as microcalcifications. Although rare, FEA is becoming increasingly diagnosed at core needle biopsy due to the improved ability of breast imaging to detect microcalcifications.
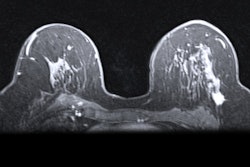
 Low-power magnification view of FEA. All images courtesy of the RSNA.
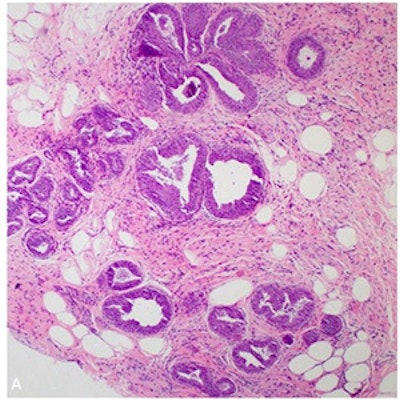
Low-power magnification view of FEA. All images courtesy of the RSNA.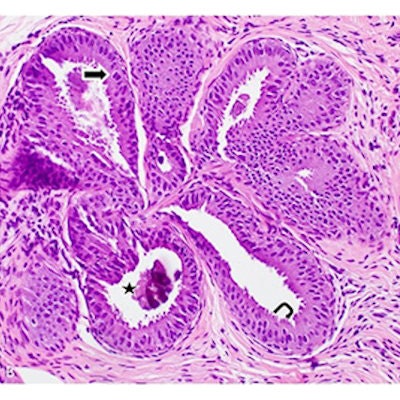 High-power magnification view of characteristic FEA features: (straight arrow) Relatively oval and monotonous nuclei, (hooked arrow) prominent apical snouts, (star) luminal calcifications.
High-power magnification view of characteristic FEA features: (straight arrow) Relatively oval and monotonous nuclei, (hooked arrow) prominent apical snouts, (star) luminal calcifications.Treatment of pure FEA can be controversial because published rates of FEA converting to cancer can vary widely. The authors conducted the review to help clarify the best treatment options.
The review included English-language studies that reported on the upgrade rate of pure FEA to cancer at surgical excision or two-year imaging follow-up. A total of 42 studies with 2,482 patients met their inclusion criteria.
Pooled analysis showed that 5% of pure FEA upgraded to cancer at surgical excision or two-year imaging follow-up. The rate was similar (4%) when Wahab and colleagues only included studies that had at least 30 cases or that used a biopsy gauge smaller than 12.
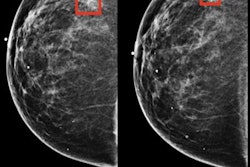
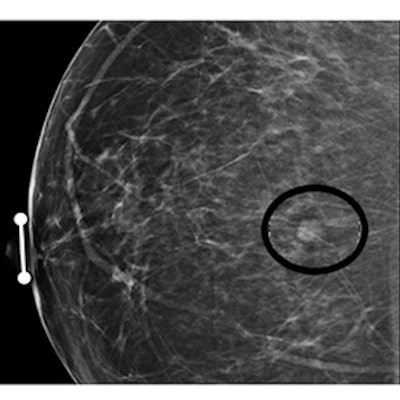
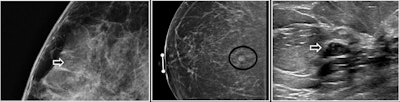 Examples of FEA on abnormal screening mammograms.
Examples of FEA on abnormal screening mammograms.When the authors only analyzed studies that reported cancer type, FEA had an upgrade rate of 1% to invasive cancer and 2% to DCIS. They also observed stable upgrade rates over time.
In addition, 17% of FEA cases occurred with atypical ductal hyperplasia, a benign breast lesion known for signaling women who are at higher future cancer risk. The researchers believe this only strengthens their recommendation for surgical excision of FEA.
"The high co-occurrence rate further supports surgical excision of pure FEA to identify these at-risk women," they wrote.
The one exception may be cases where more than 90% of the lesion is removed with a large core needle biopsy. In 11 studies that took this approach, the pooled upgrade rate was 0%.
"Use of a larger sized needle allows for nearly complete removal of calcifications because more tissue can be collected," the authors wrote. "Thus, if more than 90% of a group of calcifications is removed at CNB, these women can be closely followed with imaging."