Mammographic surveillance after breast-conserving therapy (BCT) can be improved by digital breast tomosynthesis (DBT), or in particular, by artificial intelligence (AI), according to research posted August 11 in the American Journal of Roentgenology.
In a retrospective study involving over 300 patients receiving breast-conserving therapy, a team of researchers from Yonsei University College of Medicine in South Korea found that adding DBT or mammography AI-based computer-aided detection (CAD) software to digital mammography alone led to higher accuracy for radiologists. However, AI contributed the most value in the ipsilateral breast.
"AI-CAD is a useful adjunct for reducing false-positive findings when performing post-BCT surveillance mammography," wrote the researchers led by first author Dr. Jung Hyun Yoon, PhD, of Yonsei University College of Medicine in Seoul, and senior author Dr. Hee Jung Moon, PhD, of Yonsei University Wonju College of Medicine in Wonju.
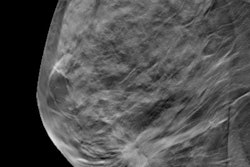
Mammograms performed postoperatively after BCT can be challenging to interpret due to postoperative distortions and hematomas, according to the researchers. As a result, they sought to investigate the potential added benefit from adjunctive use of DBT or AI-based CAD in women receiving mammography surveillance after BCT.
The study involved 314 women -- including four with bilateral breast cancer -- who underwent breast-conserving therapy followed by DBT at their institution between November 2015 and August 2018. Of the 314 women, six had breast cancer recurrence: three in the ipsilateral breast and three in the contralateral breast.
Three dedicated breast radiologists with seven, 12, and 24 years of experience, respectively, independently reviewed the images in three different sessions. They first evaluated the digital mammography exams, followed immediately by the DBT images. One month later, they assessed the mammography studies with the assistance of version 1.1 of the Insight for Mammography AI-based CAD software (Lunit).
The researchers found that both DBT and the AI-based mammography CAD software yielded higher accuracy and lower recall rates compared with digital mammography alone for both the contralateral and ipsilateral breasts. However, the AI software led to even better mean radiologist accuracy (p < 0.05) and recall rate (p < 0.001) than DBT in the ipsilateral breast.
| Performance improvement from adding DBT or AI-CAD to digital mammography | ||||||
| Contralateral breast | Ipsilateral breast | |||||
| Mammography alone | Mammography + DBT | Mammography + AI | Mammography alone | Mammography + DBT | Mammography + AI | |
| Mean accuracy | 92.5% | 96.1% | 97.1% | 88.5% | 94.8% | 97% |
| Mean recall rate | 6.6% | 2.7% | 1.5% | 11.2% | 4.1% | 1.9% |
"These findings suggest a promising role for AI-CAD in addressing the challenge of callbacks with benign results in the evaluation of the post-BCT breast," the authors wrote.
The higher accuracy did come with lower sensitivity, though. Mean radiologist sensitivity dropped in the ipsilateral breast from 66.7% on mammography alone to 22.2% on either DBT or AI-CAD (p = 0.03). Sensitivity also declined in the contralateral breast from 33.3% with mammography alone to 22.2% with DBT and 11.5% with AI, but that difference was not statistically significant.
Nonetheless, the researchers concluded that AI-CAD may help address the challenges of surveillance mammograms in patients after breast-conserving therapy.