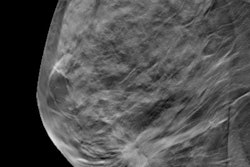
Machine-learning models could help predict which patients with ductal carcinoma in situ (DCIS) should be upstaged by using radiomic features from mammograms, according to research published January 4 in Radiology.
A team led by Rui Hou, PhD, from Duke University found that AI based on mammography radiomics is superior to using models trained in clinical criteria alone.
"This suggests potential to use imaging algorithms to improve patient care and assist in the selection of patients for clinical trials," Hou and colleagues said.
DCIS accounts for nearly 15% of all new breast cancer diagnoses. While DCIS on its own is not life-threatening, the study authors said these lesions could be precursors to invasive ductal carcinoma.
While it's standard practice to surgically remove DCIS lesions, active surveillance methods are being explored to address concerns about overtreatment. However, predicting which DCIS calcifications will progress into invasive cancers is a difficult task for radiologists.
Hou et al wanted to use a deep-learning model they developed to retrospectively look at radiomic features from mammograms to predict invasive cancers among women diagnosed with DCIS based on core biopsy findings. They focused on women who presented only with calcifications, since they could be eligible for deescalation treatment strategies such as active surveillance.
"In addition, we evaluated the use of our model in surgical treatment planning for patients undergoing surgery," the team added.
The group looked at data from 700 women with DCIS with an average age of 59 years, including 114 with lesions that were upstaged to invasive cancer at surgery. The cases were biopsied between 2008 and 2017. The women were randomly split into two groups, 400 for the training set and 300 for the testing set.
The authors extracted a total of 109 radiomic and four clinical features and tested their model by using combinations of these features. They also used fixed sensitivities and specificities in some scenarios.
The researchers found that the best combination used all radiomic features. With this, the model helped predict upstaging with an area under the curve (AUC) of 0.71.
For a fixed high sensitivity of 90%, the model had a specificity of 22%, a negative predictive value of 92%, and an odds ratio of 2.4. A high specificity of 90%, meanwhile, had a sensitivity of 37%, a positive predictive value of 41%, and an odds ratio of 5.
When using just radiomic features, the model had an AUC of 0.63. However, its performance was found to be "consistently poor" when it used clinical features only, with an AUC ranging between 0.51 and 0.57 for each individual feature.
Hou and colleagues wrote that they are continuing to use the deep learning prediction models and gathering external test data from other centers and imaging platforms. They said using such tools for risk stratification may allow for safe de-escalation of treatment in low-risk clinical settings.
"These combined efforts are aimed to allow better risk stratification, thus enabling a tractable way forward toward risk-based treatment for DCIS," they added.