Women have nearly a 7% less chance of receiving a false-positive exam from annual digital breast tomosynthesis (DBT) than conventional digital mammography after 10 years of screening, according to research published March 25 in JAMA Network Open.
A team led by Dr. Thao-Quyen Ho, PhD, from University of California, Davis also found that women had about a 2.5% lower chance of receiving a false-positive exam from biennial DBT than mammography and that older age and nondense breasts play a part in reducing false-positive probabilities.
"To our knowledge, this study is the first to estimate the cumulative probability of a false-positive short-interval follow-up recommendation after 10 years of subsequent screening, with approximately 17% of women expected to experience at least one short-interval follow-up recommendation under annual screening compared with 10% under biennial screening," Ho and colleagues wrote.
Previous research suggests that 12% of patients who undergo breast screening with digital mammography are recalled for additional workup. This team found that over one-third of these patients, or 0.53% of screening mammograms overall, result in a cancer diagnosis.
A Breast Cancer Surveillance Consortium (BCSC) study published in 2011 estimated that after 10 years of annual screening, 61% of individuals would experience at least one false-positive recall, with 7% to 9% having at least one false-positive biopsy recommendation. This study included mostly film-screen mammography and women aged 40 to 59 years.
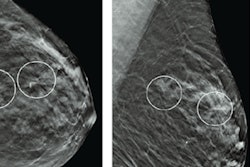
DBT has emerged over the past decade, with researchers touting its lower recall and false-positive rates. However, the researchers wrote that effective screening requires "many" examinations over multiple decades.
Ho et al wanted to find out the probability of receiving at least one false-positive result after 10 years of screening with DBT versus digital mammography in the U.S. They also looked at the cumulative probability of short-interval follow-up recommendation and biopsy recommendation for annual versus biennial screening. The decade of age and BI-RADS breast density category were also explored.
The team used data from the Breast Cancer Surveillance Consortium, which included 903,495 women and 969,055 nonbaseline screening examinations. Interpretations were performed by 699 radiologists.
| 10-year cumulative false-positive probabilities for annual and biennial DBT screening vs. digital mammography | ||||
| Mammography | DBT | |||
| Annual | Biennial | Annual | Biennial | |
| Probability of having at least one false-positive recall | 56.3% | 38.1% | 49.6% | 35.7% |
| False-positive follow-up recommendation over short interval | 17.8% | 10.5% | 16.6% | 10.3% |
| False-positive biopsy recommendation | 11.7% | 6.7% | 11.2% | 6.6% |
The study authors also found that decreases in cumulative probabilities of false-positive results with DBT versus digital mammography were largest for annual screening in women with nondense breasts. They wrote that the differences for recall ranged from -6.5% to -12.8% in favor of DBT.
They also found that older women and women with entirely fatty breasts instead of dense breasts were less likely to receive a false-positive reading no matter what imaging method was used.
In an invited commentary piece, Dr. Lydia Pace from Brigham and Women's Hospital in Boston wrote that the study's results underscore how individual characteristics such as age and breast density, may affect whether a woman will benefit from mammography screening. She added that it adds further evidence of the importance of an individualized approach to screening decisions.
"The study ... reminds us that even if we practice in a center where DBT is routinely offered, clinicians should continue to counsel patients that false-positive results are an expected outcome from mammography screening," Pace wrote.