3D printing has emerged as a disruptive technology in the healthcare field. Over the past 20 years, it has been used with great success to plan complex medical procedures, produce custom devices and instruments, and better train future clinicians.
As accessibility to the technology increases, hospitals are beginning to adopt 3D printing programs within their institutions, with the goal of decreasing 3D printing lead times and building knowledge internally.
Equal to the tremendous potential of 3D printing, there are also significant challenges to its widespread adoption. Reimbursement, lack of evidence proving efficacy, and technical limitations all contribute to this situation. One of the largest barriers to overcome is the technical know-how necessary to implement such a new technology in the existing clinical workflow.
So where should you start when considering the implementation of a 3D printing program, large or small? What does the entirety of the 3D printing process look like in a medical center? These are some questions to ask and things to take into account when considering your own 3D printing core lab.
Departmental or institutional?
Is your goal to support a single medical discipline with 3D printing? Or to provide a large-scale service institution-wide?
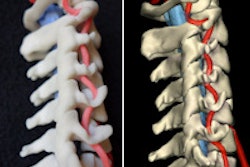
The answer to this question will determine not only the resources needed to run the lab, but also the appropriate software and hardware necessary to optimally support specific medical disciplines with 3D-printed models. Understand the modeling requirements for each discipline you are seeking to serve prior to making significant investments. Your workflow will look very different if you are building models to support congenital heart surgery, as opposed to bone models for complex craniomaxillofacial surgery.
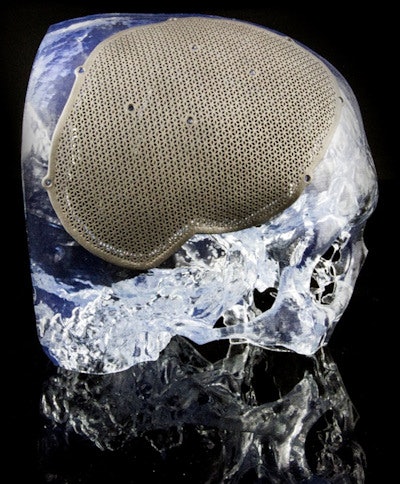 3D-printed skull defect and custom cranioplate. All images courtesy of Materialise.
3D-printed skull defect and custom cranioplate. All images courtesy of Materialise.Imaging is everything
When building patient-specific models or medical devices, great imaging is the precursor for accurate 3D models and an efficient process. CT or MRI? Contrast-enhanced or noncontrast? Each modeling application will have unique imaging requirements, so a close collaboration with your imaging departments is key.
It is also important to define the appropriate protocols as early as possible to avoid the need to rescan a patient or to work with less-than-optimal imaging. In general terms, it is best to acquire images at high resolution -- both spatial and temporal -- to achieve the best 3D printing results (thin-slice, gated imaging). Lean on the expertise of your radiologists to define optimal protocols, or reach out to the industry for recommendations.
Ordering and communication
How do surgeons indicate when they would like a model to support a procedure? Do they send an email or walk to the lab to discuss the request in person? When does it make sense to implement a more sophisticated ordering system?
There is no clear answer for this, and I wouldn't let questions like this hinder your ability to get started. Start simple and develop close working relationships with your surgeons before building a more robust system into the clinical workflow.
Software for the 3D printing workflow
Appropriate processing of your medical imaging data for 3D printing is often an overlooked part of the workflow. To optimize your workflow from DICOM image acquisition to the 3D printer, it is best to find a single software solution that addresses each step of the workflow. This will save you time and reduce headaches and errors that can arise when linking steps between software programs licensed by different vendors. Considering that the results of your modeling will be used to supplement clinical decision-making, it is also imperative to use software tools that are cleared for medical use and have U.S. Food and Drug Administration (FDA) 510(k) clearance.
As a general rule, start first by fully understanding the needs of the clinician for a specific use case for 3D-printed models. Will the model be used as a presurgical planning tool? Or will it be used for education or training?
Make sure you understand the necessary anatomy and additional landmarks needed in the model. Fully understanding the scope of the project from the beginning will ensure a useful model for the surgeon, save time in the segmentation/modeling process, and often lead to a faster build using less printing material.
Image processing
The considerations for preparing CT, MRI, or 3D ultrasound data for 3D printing are very different from traditional image processing and 3D volume-rendering techniques. Choose an appropriate software tool that has a strong combination of automated and manual segmentation functionality.
Often the cases that will benefit most from 3D printing are the most complex in terms of anatomical anomalies. This can challenge even the most sophisticated segmentation algorithms, so also find a tool that enables efficient manual intervention during segmentation when necessary.
In addition, it is useful to have a tool that can reconstruct and render your stereolithography (STL) files within the software instead of a simple STL export option. This gives you the advantage of seeing and verifying what you have created prior to 3D printing.
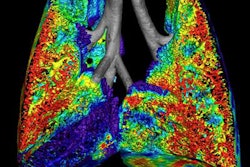
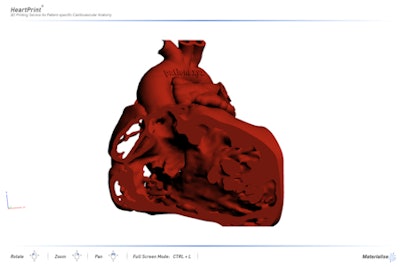
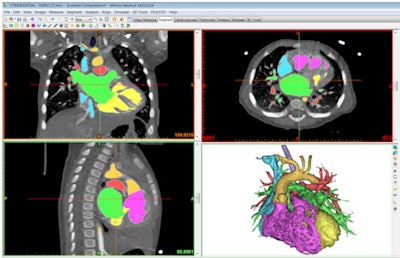 Congenital heart anatomy segmented with Mimics Innovation Suite software.
Congenital heart anatomy segmented with Mimics Innovation Suite software.3D modeling
Segmenting the medical imaging is only half of the battle. Often, the more important and labor-intensive part of the 3D printing process is the further preparation and augmentation of your segmented anatomy. This can include features such as cleaning and smoothing to remove artifacts, adding connectors to hold anatomies in the proper anatomical positions, adding thickness to represent vessel walls, cutting of the model to achieve optimal visualization, and indicating color or multiple materials.
The considerations are many. How you prepare the 3D model will determine how useful the print will be clinically, how much time and material will be required to build the part, and the feasibility of printing and cleaning the eventual model.
For example, if your surgeon requests a model to plan a repair of facial trauma, he or she may also want to understand the optimal outcome to restore cosmetics and function. For this, it would be helpful to provide a second model of the patient's anatomy mirrored across the midface to understand what the optimal outcome would look like.
For a complex heart procedure, the surgeon will want to understand the intricacies of the intracardiac anatomy or landmarks for a specific valve or vessel. This will require you to prepare the heart model with windows or cut along a split line to achieve this visualization and separate components to identify another color in the model. Each application of 3D printing will have very different 3D modeling requirements.
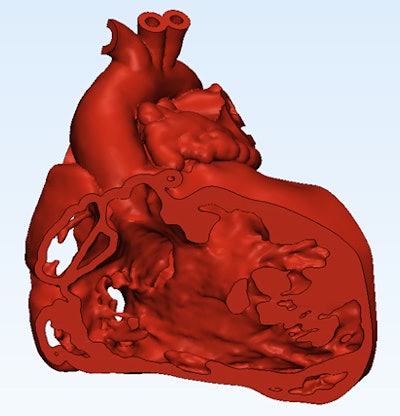 Cutaway view of the heart generated with Mimics Innovation Suite 3D modeling software.
Cutaway view of the heart generated with Mimics Innovation Suite 3D modeling software.Verification and labeling
After completing your segmentation and modeling work, you might be in a hurry to get your part on the 3D printer. However, there are opportunities to unintentionally introduce errors in the above steps.
Prior to printing, the accuracy of your final file should be verified against the original DICOM imaging. Did you oversmooth and remove a key feature from the model? Did you cut away a structure that would be an important landmark for the surgeon?
I would recommend a solution that allows the user to overlay the STL surfaces back on the DICOM data. This will allow you to verify accuracy (and convince others of it), as well as make subtle adjustments or refinements to the model.
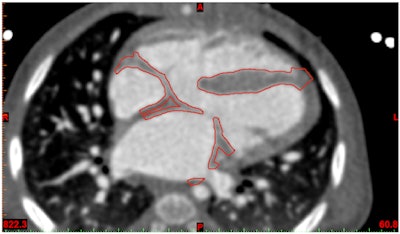 Contour verification of prepared heart model demonstrated in Mimics Innovation Suite software.
Contour verification of prepared heart model demonstrated in Mimics Innovation Suite software.Ensuring traceability of your 3D prints will also reduce the opportunity for errors with your 3D printing program. As you scale your operation and build greater volumes of models, it is critical to understand what part is coming off the printer and what case it belongs to.
To reduce the chance of mixing models or providing the wrong model to a surgeon, each anatomical model should be prelabeled with software prior to printing. Use a requisition number that will trace back to the medical records to ensure traceability of your 3D models.
You should also use labels if you create mirror images or want to clearly indicate what side of the patient the model was derived from. This will reduce the chance for operator confusion and the possibility of operating on the wrong side of the body.
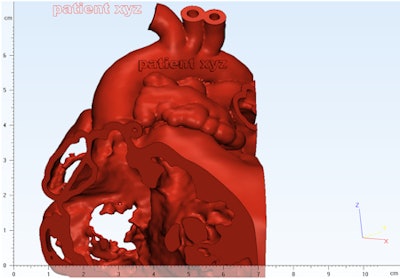 Applying a text label to a heart model using Mimics Innovation Suite.
Applying a text label to a heart model using Mimics Innovation Suite.Communication
Close collaboration between personnel is essential in this process. It is necessary to define the scope and use of the model with the surgeon or interventionist prior to starting the process, in addition to verification near the end. This can be facilitated through Web meetings or face-to-face discussion. It can also help to have a software solution capable of exporting a file format, which can be interrogated by the surgeon. It is highly unlikely that your surgeon will be able to open an STL file! Exports such as 3D PDFs can be an excellent tool for this purpose.
 3D PDF communication tool exported from Mimics Innovation Suite.
3D PDF communication tool exported from Mimics Innovation Suite.3D file fixing
The STL file format is the universal digital 3D modeling format for 3D printing. This is the file that will be fed to the 3D printer to slice and build the part.
Not all STL files are created equal. The number and quality of the triangle facets will determine the eventual quality of your printed part. You may also find very thin walls in the model that fall under the minimum resolution of your printer or that will be very brittle and tear-sensitive. It is imperative to have a robust STL diagnostic and fixing tool to ensure a successful and quality build.
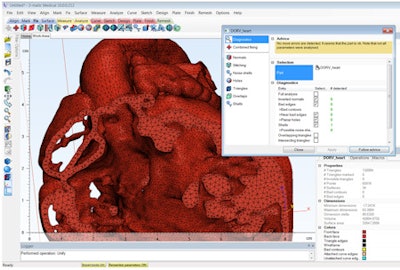 File fixing in preparation for 3D printing in Mimics Innovation Suite.
File fixing in preparation for 3D printing in Mimics Innovation Suite.3D printers: How to choose?
Insource or outsource? This is the first question you should ask. Outsourcing will allow you to minimize your upfront investment, but it is typically associated with longer lead times. Outsourcing can also be advantageous in the rapidly evolving market of 3D printers. What you buy today could soon be obsolete with better and lower-cost technology being brought to market. From a purely economic standpoint, outsourcing is often the best strategy to get started.
If you decide to invest in a printer, where should you start? 3D printers come in many different technologies, which all have their advantages. FDM, PolyJet, laser sintering, stereolithography, and binder jetting all have unique advantages for certain applications. Resolution, speed, materials, color, and of course cost are key factors you should consider. Leverage experts in the industry to understand what technology makes the most sense given your use case and budget.
In addition to understanding the best 3D printer for your program, you'll also need to understand the space required to house it. Certain printing technologies take up a very small footprint, while others may require dedicated facilities. Some machines require additional equipment to clean the models after printing or will need greater maintenance. Fully understand all of these considerations before making your choice.
 Example of a flexible 3D-printed heart model.
Example of a flexible 3D-printed heart model.Personnel and training
You will need specific skillsets to run an effective 3D printing service. Knowledge in imaging and anatomy/pathology is required for accurate segmentation. A level of engineering skill is needed to prepare your 3D models in the best way for printing. Additional resources may be needed to clean models and maintain machines.
The scale of your operation will determine the resources. Start small and lay out a plan for growth. By starting at a small scale, you can then build momentum with clinicians and administrators to support the activity.
Be sure to learn from and be trained by experts in the field. Master the process from image acquisition through 3D printing. This will ensure that you avoid common pitfalls and are operating in the most efficient way possible.
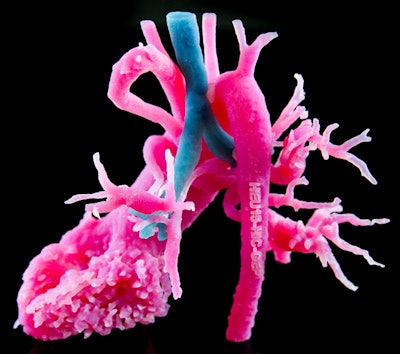 Example of a multimaterial 3D-printed model of a heart and airway anomaly.
Example of a multimaterial 3D-printed model of a heart and airway anomaly.Final thoughts
Although 3D printing as a core service in a hospital is still in its infancy, many innovative institutions have been blazing a path. Leverage the experts both in industry and among your peers who have developed similar programs. This might mean working collaboratively on a few cases as a service or visiting other established medical 3D printing facilities.
Establishing a new technology such as 3D printing can seem like an overwhelming endeavor. Taking into account the many considerations and requirements will help you develop a plan to start and grow a successful service for your institution.
Todd Pietila is a business development manager at Materialise, where he specializes in delivering 3D software and 3D printing consultancy to the healthcare field. With a background in biomedical engineering, he has spent more than six years at Materialise in various engineering roles focused on the applications of 3D printing in medicine. His current position involves working directly with healthcare providers to develop and implement 3D printing solutions into clinical practice. He can be reached at [email protected].
The comments and observations expressed do not necessarily reflect the opinions of AuntMinnie.com.