The promise of 3D-printed functional organs took a big step forward with the recent implantation of 3D-printed ovaries in mice. The bioprosthetic ovaries enabled the animals to ovulate and give birth to healthy pups, according to a study published online May 16 in Nature Communications. The mothers were even able to nurse their young.
The bioprosthetic ovaries are made of 3D-printed scaffolds that house immature eggs, and they have been successful in increasing hormone production and restoring fertility in mice, reported researchers from Northwestern University (Nat Commun, May 16, 2017).
"In this work, we investigated how scaffold pore geometry affected the growth and maturation of ovarian murine follicles as well as developed a bioprosthetic ovary that restored ovarian function in vivo in mice," wrote Monica Laronda, PhD, and colleagues. "We found that specific scaffold architectures created a 3D feel by providing appropriate depth and multiple contact sites for the ovarian follicle, which resulted in optimal murine follicle survival and differentiation in vitro."
Ovary failure common
Patients who are treated for diseases such as cancer may be left with diminished ovarian function, including experiencing early menopause or being unable to undergo puberty or maintain fertility. Meanwhile, current assisted reproductive technologies such as hormone restoration, in vitro fertilization, and ovarian transplantation do not provide long-term solutions.
3D printing offers a possible solution through the creation of a human bioprosthetic ovary that would be fully functional. As a first step, the authors investigated the creation of a bioprosthetic ovary in mice.
There have already been several reports of live births from biomaterial implants in mice, all using isolated follicles or whole ovarian tissue encapsulated in a plasma clot or similar fibrin hydrogel bead that contains growth factor components.
Hydrogel encapsulation of follicles poses several challenges, especially with respect to the size of transplants. When this work is translated to a large animal or human, the implant must house a significantly larger population of follicles than used in mice. At larger scales, diffusion limits may become a factor; therefore, future strategies must enable channels within the hydrogels to facilitate host vasculature infiltration, or include pre-embedded vasculature to sustain follicle viability and circulate follicular hormones.
Finally, ovaries are heterogeneous organs that compartmentalize different follicle pools into the cortex and medulla regions that have varying stiffness, according to the authors. As a result, the ability to compartmentalize will be crucial to providing long-term function. What's needed is a strategy to produce a construct of spatially varying material properties for long-term function --requirements that 3D printing can provide.
3D printing
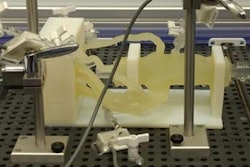
To create the ovaries, investigators needed to use gelatin, which is a biological hydrogel made from broken-down collagen that is safe to use in humans. They knew whatever scaffold they created needed to be made of organic materials that were rigid enough to be handled during surgery and porous enough to naturally interact with the mouse's body tissues.
The researchers found a gelatin temperature that allows it to be self-supporting and not collapse, enabling it to be used to build multiple layers. They believe their discovery of this process is novel, and this geometry was key to the creation of follicles that were able to survive in the ovary.
After removing the ovaries of female mice and replacing them with bioprosthetic ovaries, the mice were able not only to ovulate but also to give birth to healthy pups. The moms were even able to nurse their young.
"This is the first study that demonstrates that scaffold architecture makes a difference in follicle survival," said senior author Ramille Shah, PhD, an assistant professor of materials science and engineering, in a statement. "We wouldn't be able to do that if we didn't use a 3D printer platform."
What does the research mean for humans? It could help restore fertility and hormone production in women who have undergone cancer treatment as an adult, or for those who survived cancer in childhood and now have increased risks of infertility and hormone-based developmental issues.
"This research shows these bioprosthetic ovaries have long-term, durable function," added co-author Teresa Woodruff, PhD, a reproductive scientist and director of the Women's Health Research Institute. "Using bioengineering, instead of transplanting from a cadaver, to create organ structures that function and restore the health of that tissue for that person is the holy grail of bioengineering for regenerative medicine."