Preoperative simulation with 3D printing models can improve surgical results for treatment of old and complex tibial fractures, leading to faster and more personalized procedures with less intraoperative blood loss and fluoroscopy time, according to research published online April 8 in Scientific Reports.
In a retrospective analysis, a team of researchers led by Sheng Shen and PeiZhao Wang of Henan Orthopedic Hospital in Henan, China, found that a group of patients that had received surgeries planned from 3D-printed fracture models had better overall results compared with patients whose procedures were planned solely from preoperative CT images.
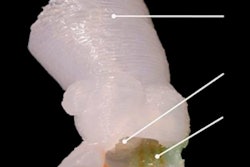
"The results showed that an individualized solid model of the fracture with an equal ratio to the actual fracture produced by 3D printing techniques can help surgeons accurately observe and analyze the morphology and displacement of fragments," the authors wrote. "Meanwhile, through preoperative surgical simulation on the 3D printing model, the reduction steps of the fragments, placement, and pre-reshaping of the plates, and the measurement of the screw length can be accurately determined and recorded."
Challenging surgeries
Mostly caused by high-energy injuries, complex tibial plateau fractures are often accompanied with the collapse of the tibial plateau surface, displacement of the comminuted fragments, and knee joint dislocation, according to the researchers. Without proper treatment, complications such as postoperative wound infection, skin necrosis, joint deformity, and traumatic arthritis are very likely.
Furthermore, "if complex tibial plateau fractures develop into old fractures, they become more challenging for orthopedic surgeons to optimize the surgical procedures to improve the operation efficiency and to reduce postoperative complications," the authors wrote.
To see if 3D printing could improve on the current use of preoperative x-ray and CT images for surgical planning, the researchers enrolled 42 patients with old and complex tibial fractures in a retrospective study. Of these, 20 patients had treatments planned with 3D models and 22 received conventional planning based on preoperative CT. The researchers found no significant difference among the groups in the number of plates used and the choice of surgical approach. The mean patient follow-up time was 25.4 ± 6.9 months.
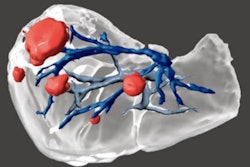
For patients receiving 3D printed models, CT DICOM data were imported into version 10.01 of the Mimics image processing software (Materialise) to construct a 3D digital model of the fracture. This model was then imported to a 3D printer (Watson Med) to produce a patient-specific fracture model with a 1:1 ratio of the actual fracture.
| Use of 3D printing for treatment of tibial plateau fractures | ||
| Conventional planning group | 3D printing group | |
| Mean intraoperative time | 152.5 ± 29.6 minutes | 127.3 ± 8.03 minutes |
| Mean intraoperative blood loss | 266.4 ± 49.04 mL | 202.5 ± 32.3 mL |
| Mean number of intraoperative fluoroscopy scans | 11 ± 1.83 | 6.55 ± 1.09 |
| Rate of excellent fracture reduction at six months follow-up* | 45.5% | 75% |
| Complication rate | 31.8% | 15% |
| Mean Hospital for Special Surgery (HSS) Knee score at final follow-up evaluation | 79.05 ± 6.75 | 85.05 ± 7.67 |
| Rate of patients with HSS Knee score results categorized as excellent at final evaluation | 45.5% | 70% |
The improvements in operation time, blood loss, and amount of fluoroscopy were all statistically significant (p = 0.001), as were the rate of excellent fracture reduction (p = 0.05) at six months and the better mean HSS Knee score at final follow-up (p = 0.003). However, the difference in the rate of patients who produced an excellent HSS score did not reach statistical significance between the groups (p = 0.083).
More accurate, personalized treatment
The operation time and intraoperative blood loss were lower in the 3D printing planning group because the anatomical reduction and fixation of the fragments can be performed during the operation based on the preoperative planning design, according to the researchers.
"Postoperative follow-up results also showed that the articular surface and plateau height remained viable, and the excellent rate of function was higher than that in the conventional planning group," they wrote. "Taken together, the results suggest that 3D-printed fracture models facilitate the treatment of old and complex tibial plateau fractures via a more accurate and personalized approach, thus confirming its effectiveness for this type of fracture."
The researchers acknowledged, however, that this approach still needs to be prospectively assessed via a randomized controlled study.