The future is now for 3D imaging technologies such as cinematic rendering, 3D printing, simulation training, virtual reality, and augmented reality, according to a June 26 presentation at the virtual annual meeting of the Society for Imaging Informatics in Medicine (SIIM).
"These are really exciting times to look into 3D technologies because of custom and personalized medicine, as well as value-based care," said Dr. Ramin Javan of George Washington University (GWU) Hospital in Washington, DC.
Advancements in 3D technologies have facilitated personalized and targeted medical care, better patient understanding and satisfaction, and multispecialty and multi-institutional collaboration, Javan said.
"As gateways of imaging, [radiology departments] can help consolidate these 3D techniques in hospitals and academic institutions," he said.
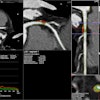
Cinematic rendering
Emerging in recent years due to advances in gaming technologies and new powerful processors, cinematic rendering creates a photorealistic appearance on images by accounting for the complex reactions of photos, according to Javan. This enables the incorporation of lighting, shading, focus points, and specular reflection.
Current cinematic rendering applications include presurgical planning, interdisciplinary consulting, patient counseling, and anatomy education, Javan said. Javan's institution uses syngo.via software (Siemens Healthineers) for cinematic rendering.
"There is ongoing research still in determining whether clinicians receive this well and adopt it ... and whether there's any improved depth and shape perception in three dimensions, and whether it's effective educationally," he said.
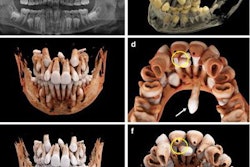
3D printing
3D printing offers a host of benefits, including improved anatomical understanding and better interdisciplinary team communication, according to Javan. It also enables customized educational tools, as well as opportunities in research and public relations. What's more, 3D printing has been shown in recent studies to reduce operating room time, errors, and revision rates, he added. It can also increase patient satisfaction.
At 3D printing labs, DICOM images need to be processed and segmented using free or commercial segmentation software that's compatible with 3D printing, according to Javan.
"This can all be done by one person, or ideally, it can be primarily done by a technologist and secondarily done and fine-tuned by a radiologist," he said.
Eventually, a stereolithography (STL) file is created, which could then be outsourced to a company or an institution that specializes in 3D printing. Or it could be printed in-house.
"If it's done in-house, an engineer or medical team has to be able to process this model, which eventually needs to be prepared for clinical use," he said.
Javan said that in terms of image acquisition, the most important thing is that thin slices are needed for CT/CT angiography exams (0.6-1 mm) and MR/MR angiography (0.5-1 mm). Freeware segmentation software options include Slicer 3D, Meshmixer, and Meshlab; a free educational license is also available for Autodesk 3D Studio.
GWU utilizes software from Materialise, which is available on an annual commercial license.
Segmentation can be outsourced, but this can be quite expensive, Javan said. Graphic artists could also be hired as well to perform segmentation.
Outsourcing or in-house?
It's important to consider the costs of outsourcing 3D printing versus buying your own printer. 3D printers can range in price from $2,000 to $250,000. Outsourcing of 3D printing can range from $200 to $3,000 per model, however.
"Basically, what it comes down to is if you do a lot of models, then it's worth it to get a printer," he said. "If you only do a few, it's probably best to do outsourcing."
3D printing materials are another important consideration, Javan said. Options include the following:
- Z-corp powder binding: A fragile, drillable, and radiodense gypsum-based material that can be used as a CT/fluoroscopy phantom and for orthopedic and calvarial applications. Price range: approximately $200-$800.
- Laser sintering: A durable, opaque, and rigid material that can be suitable for orthopedic and spine applications, as well as surgical guides. Price range: approximately $200-$1,000.
- Stereolithography: Liquid that's cured with ultraviolet light and has transparent and rigid properties that are useful for cardiac, vascular, and craniomaxillofacial applications. Price range: about $400-$1,500.
- Polyjet: A multimaterial printing technique that can use a semitransparent flexible material and/or multiple rigid, colored materials. It can be utilized in cardiac, vascular, and oncology applications, as well as for multiorgan models. Price range: about $500-$3,000.
- HP JetFusion: Can produce colorful, rigid models via multihead powder-jetting technology for use in cardiac, vascular, craniomaxillofacial, and educational applications. Doesn't require support structures. Price range: about $400-$1,500.
3D printing clinical applications
The main clinical applications include cardiovascular, musculoskeletal, craniomaxillofacial, and gastrointestinal/genitourinary, Javan said. He noted that the RSNA's 3D Printing Special Interest Group (SIG) has published a white paper that offers guidelines for medical 3D printing and appropriateness for clinical scenarios.
"The appropriateness criteria are very useful because it allows you to look at what types of pathologic conditions are useful to be considered for 3D printing," Javan said.
Also, current procedural terminology (CPT) category III codes -- 0559T, 0560T, 0561T, and 0562T -- have been released in the last couple of years for 3D printing.
3D printing educational applications
3D printing can be utilized in educational applications to show complex anatomy and to produce interventional phantoms for simulation training for procedures such as CT or ultrasound-guided interventions, vascular interventions, or surgical simulations, according to Javan.
3D printing can be used to support interdisciplinary communication. For example, a 3D-printed mesh-like brain cortex based on MRI could be used for communication between neuroradiologists, epileptologists, and neurosurgeons to go over electroencephalogram (EEG) deep electrode and strip placement planning, Javan said.
Simulation training
Simulation training is another application for 3D imaging, both from a surgical and interventional standpoint, as well as for software simulation, Javan said. For example, when Javan was a medical student, he created a video game designed to help users to understand complex anatomy in 3D.
"Basically it's predicated on the concept that when you play in these environments, it's another way for you to understand these 3D correlations," Javan said.
3D printing can be used to produce interventional phantoms for practicing image-guided procedures. It can also be utilized to create surgical models.
VR and AR
Virtual reality (VR) has many applications in radiology and is becoming more and more commonly used for surgical planning, trainee education, patient retention, and therapy for phobias, according to Javan. He said that his institution uses Surgical Theater's VR visualization platform.
Another 3D technology is augmented reality (AR), which is a superimposition of a patient's cross-sectional imaging onto their anatomy that can be viewed on a headset. GWU utilizes OpenSight software (Novarad) along with a Hololens head-mounted display (Microsoft).
"It's a quite exciting technology... and you can scroll through the images while you're looking at the patient," he said.
Researchers at GWU assessed the use of AR for localizing the pedicle spine. They found that it was pretty accurate, even when medical students were using the platform, Javan said. It has also been utilized for a few cases to support surgical stabilization of rib fractures using CT images.