A deep-learning model can generate "super-resolution" synthetic brain MR images from portable MRI scanners, enabling automated quantitative morphometry on these low-field-strength systems, according to a study published November 8 in Radiology.
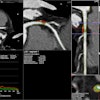
In a proof-of-concept study, a group led by Juan Eugenio Iglesias, PhD, of Massachusetts General Hospital in Boston trained a convolutional neural network (CNN) to synthesize images with 1-mm isotropic spatial resolution images from lower-resolution T1-weighted and T2-weighted brain images generated on a 0.064-tesla portable MRI scanner. In testing, the automated morphometry measurements on the synthetic images correlated highly with measurements on actual 1-mm isotopic images from high-field strength 1.5- to 3-tesla scanners.
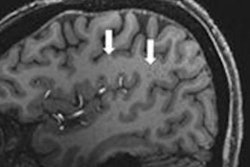
Portable, low-field-strength MRI has the potential to transform neuroimaging in a point-of-care setting. For example, depicting intracerebral hemorrhage and multiple sclerosis lesions, according to the authors. However, it's limited by low spatial resolution and low signal-to-noise ratio compared with high-field-strength MRI.
Interest has grown in artificial intelligence (AI) approaches that might help augment image quality to extract more information from scans while maintaining accuracy. Morphometry of low-field strength MRI would substantially extend its use for research and clinical neuroimaging, scientists say.
In response, Iglesias et al developed LF-SynthS, a technique for training a CNN to generate synthetic images from low-field-strength image data. To test the model, they utilized automated segmentation tools on both the synthetic images and actual images acquired on high-field-strength systems in 24 patients who had presented with neurologic symptoms.
When the researchers compared the quantitative morphometric assessments on each type of image, they found high correlations between the synthetic images generated by the algorithm and actual high-field-strength images. Volumes correlated between synthetic image datasets based on low-field-strength MRI at 0.064 T and high-field-strength T1-weighted MPRAGE datasets for multiple brain regions, even for smaller regions that are difficult to segment (e.g., the hippocampus: r = 0.85; p < 0.001).
In an accompanying editorial, Dr. Birgit Ertl-Wagner, PhD, and Dr. Matthias Wagner of the Hospital for Sick Children in Toronto noted that the algorithm is an exciting technical development.
"Future studies with larger sample sizes and a variety of brain pathologic findings will be needed to demonstrate the clinical value of the method and to ascertain those pathologic findings in the brain will not be filtered away or artificially created," wrote Ertl-Wagner and Wagner. "Nevertheless, this technical development study demonstrates the potential to go low on field strength and aim high for spatial and contrast resolution using artificial intelligence."