A new quantitative CT (QCT) technique offers hope that osteoporosis scans could someday be performed passively -- and automatically -- from abdominal CT scans acquired for other clinical purposes, according to researchers from the U.S. National Institutes of Health (NIH) in Bethesda, MD.
The research could potentially open a window to broad, population-based screening and treatment for osteoporosis, helping to prevent fractures without the need for additional imaging studies or radiation. The study was presented at the 2009 RSNA meeting earlier this month.
Osteoporosis and osteopenia are huge concerns for older individuals, particularly women, who suffer approximately 80% of the half-million or so fractures attributed to the conditions annually in the U.S.
While dual-energy x-ray absorptiometry (DEXA) is a well-established method of identifying patients at risk in order to treat them before a fracture occurs, its use is limited by the need for a separate office visit and scan. Quantitative CT bone densitometry has also been validated as a precise method of assessing bone health and risk of osteoporosis, but it requires a separate phantom scan and lacks the volume of empirical data that has been produced by years of acquiring DEXA scans in large populations at risk.
At the RSNA conference, researchers presented a new automated method of acquiring QCT densitometry that can be performed passively in patients undergoing abdominal CT.
"As you know, quantitative CT is not very frequently employed compared to other types of abdominal CT scans," in part due to the need for an external reference scan to validate the results, said Dr. Ronald Summers, Ph.D., senior investigator and staff radiologist at the NIH. "It has been my long-term goal to develop techniques in which we can make routine bone mineral density assessments from normal abdominal CT scan data," he said.
Two-in-one scans?
Providing two exams in one for this application is an attractive scenario, considering that many conditions requiring abdominal CT occur in older individuals who may also suffer from low bone mineral density. For example, "osteoporosis and colorectal polyps occur more frequently in older people," said Summers, who also leads virtual colonoscopy research efforts at NIH.
The new study, led by Dr. Nicolai Baecher, a research trainee in Summers' lab, along with Jianhua Yao, Ph.D., Jiamin Liu, Ph.D., Dr. Suvimol Hill, and Summers, aimed to "validate software that is fully automated to estimate bone mineral density with the ultimate goal of applying this to routine abdominal CT without the use of an external phantom," Summers said.
The cohort consisted of 17 consecutive women (mean age, 54 years; range, 46-68) who underwent QCT and had a reported bone mineral density (BMD) < 200 mg/cc. All images were acquired on a 64-detector-row scanner (LightSpeed, GE Healthcare, Chalfont St Giles, U.K.) using 2.5-mm collimation, 120 kVp, and 100-200 mAs.
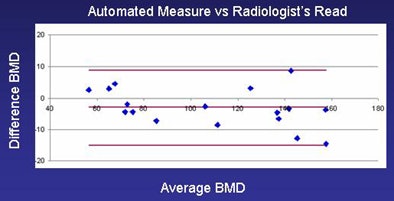 |
| Bland-Altman plot comparing fully automated method and radiologist's read. Software plot shows 95% limits of agreement comparing the average BMD of the two techniques to the difference between the two techniques, revealing a bias of -3.1 ± 12 mg/cc. Converting the BMD measurements to standard T-scores for osteoporosis assessment showed that all seven osteoporotic patients were correctly classified using the automated technique. All images courtesy of Dr. Ronald Summers, Ph.D. |
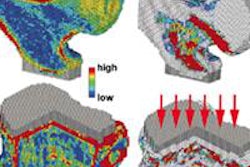
Using the CT images, the software automatically places regions of interest (ROI) over vertebral trabecular bone, fat, and muscle at the midvertebral level, he said.
"The spinal column is automatically identified ... and the L1 and L2 vertebral bodies are then identified and segmented automatically by the software without any human intervention," Summers explained. "We then remove the cortical bone from the segmented area of interest by means of mathematical erosion; then we can measure mean CT values within the central segmented region."
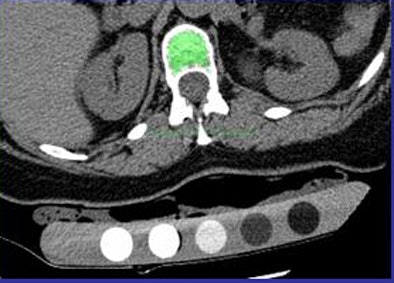 |
| Automated BMD software automatically identifies the spinal region and labels L1 and L2 vertebral bodies, segmenting them automatically. Mathematical erosion is applied to remove the cortical bone. Mean CT values are then computed within the region, and the mean of L1 and L2 CT attenuation used to compute BMD. |
The group designed a global calibration scale based on phantom results and clinical cases to provide a reference for the results in individual patients; then calcium scoring software was used to convert attenuation values to BMD scores.
Two types of validation were performed by comparing automated BMDs to manual measurements. First, the researchers used manual ROIs to estimate BMD using linear regression against an external reference phantom. Second, they used a radiologist's prospective measurements of the BMDs using commercially available software (Mindways Software, Austin, TX).
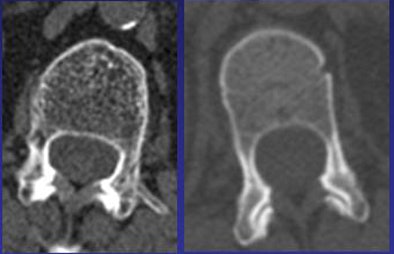 |
| QCT images show osteoporotic L1 vertebral body (left, 55 mg/cc, CT attenuation 46 HU) compared to normal subject (right, 165 mg/cc, CT attenuation 207 HU). |
The three BMD estimates were then compared using linear regression. T-scores were calculated from both the automated and prospective BMDs. T-scores were categorized based on WHO criteria for the presence of osteoporosis in each subject. Finally, Bland-Altman analysis was used to determine the 95% limits of agreement, Summers said.
The results showed excellent correlation (r2) between the fully manual method and the radiologist's read (96%, p < 0.0001); between the fully manual method and fully automated method (93%, p < 0.0001); and between the fully automated method and the radiologist's read (98%, p < 0.0001).
The Bland-Altman 95% limits of agreement comparing the automated method and the radiologist's read were -3.1 ± 12 mg/cc. Based on T-scores and World Health Organization (WHO) criteria, the method correctly classified all seven osteoporotic patients.
"The fully automated method showed excellent correlation to manual measurements of BMD and correctly classified cases of osteoporosis," Summers concluded. "It is my hope that with further validation this may allow BMD assessment without a reference scan when low BMD is suspected -- and for those who receive abdominal CT."
An audience member at the RSNA presentation noted that WHO empirical data are based on DEXA, not QCT scans, one of several reasons why "no one has proven that osteoporosis can be diagnosed by CT."
Summers agreed that historical data are lacking for QCT, but added that using the modality to perform BMD testing in patients who undergo abdominal CT scans could potentially produce the data needed for more robust validation.
By Eric Barnes
AuntMinnie.com staff writer
December 28, 2009
Related Reading
Secondary causes of bone loss may be missed in breast cancer, August 20, 2009
MDCT holds promise for advanced osteoporosis scan, April 6, 2009
More evidence for atherosclerosis and bone loss link, February 18, 2009
Flat-panel CT finds early signs of bone damage in anorexics, December 9, 2008
UCSF adds bone mineral density test to VC colon screening, December 3, 2008
Copyright © 2009 AuntMinnie.com