An advanced visualization technique utilizing curved maximum intensity projections (MIPs) that parallel the inner table of the skull may be able to significantly improve sensitivity for detecting thin epidural and subdural hematomas, according to an Austrian article published in Radiology.
Curved MIPs increased mean detection rates of thin subdural hematomas from 20% to 80% in a retrospective study involving four radiologists and 314 patients. Furthermore, the images required a significantly shorter reading time, according to a research team led by Dr. Helmut Ringl of the Medical University of Vienna.
"Together with the curved MIPs of the skull, these two advanced visualization methods bear the potential to enhance the interpretation of cranial CT images of patients suspected of having traumatic brain injury in terms of time, achieved sensitivity, and required experience," the authors wrote. "We therefore recommend using this method, in addition to reading transverse sections, in routine clinical practice in patients suspected of having traumatic brain injuries."
The gold standard
Thanks to its ability to demonstrate the presence or absence of intracranial hemorrhage, unenhanced cranial CT is the gold standard for evaluating traumatic brain injury. However, the epidural and subdural spaces can be partially masked on these studies by blooming and partial-volume artifacts.
And even if the so-called "blood window" is used in addition to the "standard brain window" on cranial CT, detecting small or thin hematomas is still challenging and time-consuming, even for experienced radiologists, according to the researchers (Radiology, May 2013, Vol. 267:2, pp. 522-530).
As a result, the Austrian team developed a curved MIP algorithm that unfolds the 3D structure of the meningeal spaces on CT data into four images that are optimized for the detection of meningeal hematomas. For both the skull vault and the skull base, "two curved MIPs were reconstructed: a 3-mm-thick, curved MIP that provides sharp visualization of the epidural and subdural spaces and a 20-mm-thick, curved MIP that covers most of the subarachnoid space as well as the cortex of the brain."
These images are similar to a map of the Earth's sphere that is projected onto a planar image, according to the authors.
"The algorithm is designed to show even very thin or small hematomas at a glance to ease and accelerate the detection process by using thin-section curved [MIPs] of the meningeal spaces," they wrote.
The software, which was developed by lead author Ringl in the Visual Basic coding language, segments and reconstructs all four images in about 20 seconds per patient. After being saved as DICOM images with 12-bit grayscale information at a resolution of 1,600 x 1,200, the reconstructions are then transferred back to the institution's PACS for reading and interpretation.
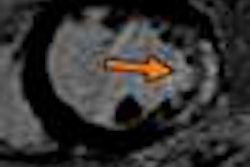
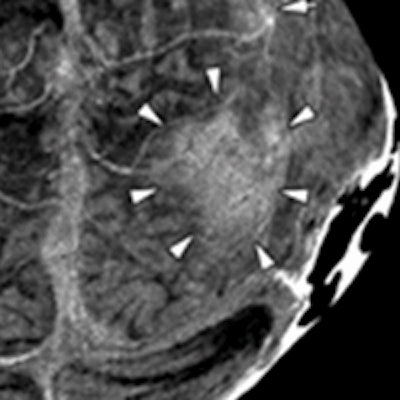
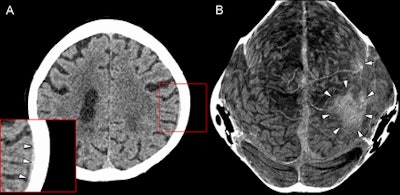 Figure A is a transverse section of a cranial CT image from a 58-year-old woman with a thin subdural hematoma (arrowheads) in the left parietal and temporal region. Lower left corner shows magnification. Figure B is a thin curved MIP of the skull vault. Arrowheads point to the large hematoma, while the single arrow in the left frontal region refers to a smaller hematoma. Image courtesy of Radiology.
Figure A is a transverse section of a cranial CT image from a 58-year-old woman with a thin subdural hematoma (arrowheads) in the left parietal and temporal region. Lower left corner shows magnification. Figure B is a thin curved MIP of the skull vault. Arrowheads point to the large hematoma, while the single arrow in the left frontal region refers to a smaller hematoma. Image courtesy of Radiology.Retrospective evaluation
The researchers sought to retrospectively assess the intracranial hematoma detection rate with their technique in comparison with the commonly used approach of reading only transverse CT sections.
The study included 314 consecutive patients who received a CT scan for cranial trauma between October 2008 and February 2009. Of the patients, 151 were performed on a Somatom Sensation Cardiac 64 scanner (Siemens Healthcare) with the institution's routine CT protocol for suspected acute head trauma. The remaining 163 patients were scanned using a Somatom Sensation Open (Siemens) system.
The four readers participating in the study consisted of two residents with two years of experience in reading body CT images and no experience in reading cranial CT studies, as well as two board-certified radiologists with seven and 10 years of experience, respectively, in interpreting cranial CT exams.
While the readers were aware of the presence or absence of hematoma and the history of head trauma of each patient, they were blinded to the extent of trauma and all other clinical information. Patients were divided into two groups consisting of 157 patients.
In each group, one inexperienced radiologist and one experienced radiologist read only the transverse sections, while the other inexperienced radiologist and experienced radiologist read only the curved MIP reconstructions. This prevented possible recognition of patients or interaction of findings, according to the authors.
For the purposes of the study, a consensus reading by two senior radiologists with 20 years of experience in reading cranial CT studies served as the reference standard.
Faster, more effective results
Mean reading times for hematoma detection were three to five times shorter (p < 0.001) when using curved MIPs. Overall, readers detected 193 (80%) of 242 lesions on transverse sections and 200 (83%) of 242 using curved MIPs. The differences between overall hematoma detection rates were not statistically significant, but they were significant for finding thin hematomas (< 3 mm thickness).
| Mean detection rate for thin hematomas | |||||
| Transverse sections | Curved MIPs | ||||
| Residents | 15% (3 of 20) | 85% (17 of 20) | |||
| Board-certified radiologists | 25% (5 of 20) | 80% (16 of 20) | |||
| Overall | 20% (8 of 40) | 83% (33 of 40) | |||
The differences for each sets of readers was statistically significant (p < 0.001).
"Curved MIPsof the meningeal spaces may shorten detection time for epidural and subdural hematomas, increase sensitivity (especially for thin hematomas), and reduce the required operator experience for detection," the authors wrote. "In addition, this visualization tool considerably enhances the detection rate for inexperienced radiologists and brings it closer to the rate seen with experienced radiologists, especially for thin hematomas."