Body composition analysis on CT exams can identify ovarian cancer patients who are more likely to have complications related to chemotherapy, according to research presented at ECR 2022 Overture.
In a retrospective study involving 69 ovarian cancer patients, a team of researchers led by Dr. Stefania Rizzo of the Imaging Institute of Italian Switzerland in Lugano, Switzerland found statistically significant associations for three CT body composition measures with chemotoxicity from neoadjuvant chemotherapy. This information could then be used clinically to adjust chemotherapy doses and to enable interventions such as recommending exercise and nutritional adjustments prior to surgery.
"In ovarian cancer patients, CT-derived body composition profiling may be associated with complications related to chemotherapy," Rizzo said.
Ovarian cancer is the fifth-highest cause of cancer death for women in developed countries. Currently, the standard treatment is primary cytoreductive surgery with complete resection of all macroscopic disease, followed by adjuvant platinum-based chemotherapy, according to Rizzo.
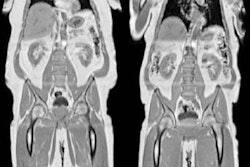
Although body surface area has generally been utilized to determine chemotherapy dosing, this approach fails to detect differences in quantity and proportion of skeletal muscle and fat tissue, Rizzo said. However, CT -- a regular component in the standard management of ovarian cancer patients -- is considered an appropriate gold standard for noninvasive assessment of muscle quantity.
In their study, the researchers sought to assess associations between quantitative measures of body composition profiling on CT exams with chemotherapy-related complications. They also wanted to evaluate for any association between sarcopenia with complications and to determine if there are any differences in body composition profiling at baseline and after neoadjuvant chemotherapy.
The researchers included patients from their institution with a first diagnosis of ovarian cancer between February 2011 and March 2020. Next, they recorded clinical data including the following: patient age, body mass index, International Federation of Gynaecological Oncologists (FIGO) cancer stage, whether or not they received neoadjuvant chemotherapy, dose reduction compared to first cycle, premature discontinuation of chemotherapy due to toxicity, cycle delays of more than two weeks due to chemotherapy-induced adverse events, and date of last contact and/or date of death to calculate overall survival.
The 69 patients in the study had an average age of 65 and a body mass index of 24.9. Most were either FIGO stage IIIC (55% of patients) or stage IV (29% of patients).
Twenty-five patients received neoadjuvant chemotherapy. Of these, nine (13%) had early discontinuation of chemotherapy, and eight (12%) had cycle delays of more than two weeks.
Using version 5.0 of the Slice-O-Matic software (Tomovision), the researchers extracted skeletal muscle area, skeletal muscle density, subcutaneous adipose tissue, and visceral adipose tissue data from an axial CT image at the level of the L3 vertebrae.
The researchers found three statistically significant associations between body composition measures and chemotherapy complications:
- Mean skeletal muscle density: Odds ratio of 0.92 for cycle delays of more than two weeks (p = 0.007).
- Skeletal muscle area: Odds ratio of 1.03 for early discontinuation of chemotherapy (p = 0.036)
- Visceral adipose tissue: Odds ratio of 1.01 for cycle delays (p = 0.044)
However, the researchers did not find any significant changes in body composition measures after chemotherapy. They also did not identify any associations between body composition measures and overall survival.
Nonetheless, these body composition measures could be used clinically to adapt chemotherapy doses to decrease the risk of complications, according to Rizzo. Surgeons can also appreciate this information.
"If [the surgeons] give nutritional support to patients before surgery, then they have a higher outcome right after surgery," Rizzo said. "They know that it works."