A group in the Netherlands has built a radiomics model using FDG-PET scans that predicts disease-free survival odds in patients with relapsed or refractory (R/R) classical Hodgkin's lymphoma (cHL), according to a study published September 20 in Blood Advances.
Ultimately, the model can identify a high-risk group of patients who could benefit from new treatment approaches, wrote lead author Julia Driessen, a doctoral student at the University of Amsterdam, and colleagues.
"We identified a subgroup of high-risk R/R cHL patients with inferior [progression-free survival] and overall survival in whom novel therapies should be considered," the group wrote.
Relapsed or primary refractory classical Hodgkin lymphoma can be cured in only about half of patients, typically with salvage chemotherapy and autologous stem cell transplants, the authors explained. Thus, prognostic factors that can help identify which patients are at higher risk are essential, they noted.
Since PET scans are already used in clinical practice in these patients, a prediction model based on radiomics features culled from the imaging could help identify these patients and ultimately help guide treatment decisions in clinical practice, the group wrote.
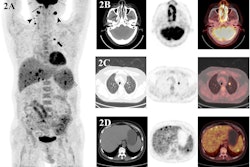
To build the model, the researchers extracted metabolic tumor volume (MTV) and several novel radiomics features representing differences in cancer lesions, as well as standard radiotracer uptake values (SUVs), from baseline PET scans in 113 patients.
They then tested the model's predictions in an independent external cohort of 69 patients who had participated in a previous clinical trial. All of the patients had been eligible for stem cell transplants and had biopsy-proven cHL and the PET-CT scans were performed before the start of salvage therapy.
The primary endpoint was whether the model could predict three-year progression-free survival (PFS) in this group.
According to the findings, the model stratified the cohort into low- and high-risk patients, with patients identified as high-risk having a 38.5% chance of three-year PFS compared with low-risk patients (75%). In addition, overall survival was also significantly better in the low-risk group based on the model's predictions.
Ultimately, several previous studies have developed prognostic models based on clinical characteristics and patient response to stem cell transplantation, but models for risk profiling at baseline, before starting second-line treatment, are scarce, the authors wrote. Thus, their baseline model has the advantage of being able to preselect patients with high-risk disease and change therapy upfront, they suggested.
"This model calculates a PET-based risk profile and can be applied to develop risk-stratified treatment strategies for R/R cHL patients," the group wrote.
The full study can be found here.