J Nucl Med 2001 Aug;42(8):1198-215
Radioguided sentinel lymph node biopsy in breast cancer surgery.
Mariani G, Moresco L, Viale G, Villa G, Bagnasco M, Canavese G, Buscombe J,
Strauss HW, Paganelli G.
The concept of sentinel lymph node biopsy in breast cancer surgery relates to
the fact that the tumor drains in a logical way through the lymphatic system,
from the first to upper levels. Therefore, the first lymph node met (the
sentinel node) will most likely be the first to be affected by metastasis, and a
negative sentinel node makes it highly unlikely that other nodes are affected.
Because axillary node dissection does not improve prognosis of patients with
breast cancer (being important only to stage the axilla), sentinel lymph node
biopsy might replace complete axillary dissection to stage the axilla in
clinically N0 patients. Sentinel lymph node biopsy would represent a significant
advantage as a minimally invasive procedure, considering that, after surgery,
about 70% of patients are found to be free from metastatic disease, yet axillary
node dissection can lead to significant morbidity. Furthermore, histologic
sampling errors can be reduced if a single (sentinel) node is assessed
extensively rather than few histologic sections in a high number of lymph nodes
per patient. Although the pattern of lymph drainage from breast cancer can be
variable, the mammary gland and the overlying skin can be considered as a
biologic unit in which lymphatics tend to follow the vasculature. Therefore,
considering that tumor lymphatics are disorganized and relatively ineffective,
subdermal and peritumoral injection of small aliquots of radiotracer is
preferred to intratumoral administration. (99m)Tc-labeled colloids with most of
the particles in the 100- to 200-nm size range would be ideal for radioguided
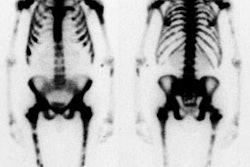
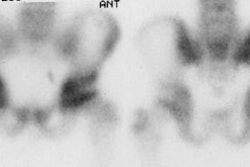
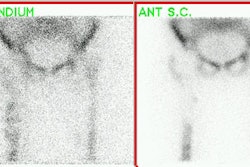
sentinel node biopsy in breast cancer. Lymphoscintigraphy is an essential part
of radioguided sentinel lymph node biopsy because images are used to direct the
surgeon to the site of the node. The sentinel lymph node should have a
significantly higher count than that of background (at least 10:1
intraoperatively). After removal of the sentinel node, the axilla must be
reexamined to ensure that all radioactive sites are identified and removed for
analysis. The sentinel lymph node should be processed for intraoperative frozen
section examination in its entirety, based on conventional histopathology and,
when needed, immune staining with anticytokeratin antibody. The success rate of
radioguidance in localizing the sentinel lymph node in breast cancer surgery is
about 94%--97% in institutions where a high number of procedures are performed
and approaches 99% when combined with the vital blue dye technique. At present,
there is no definite evidence that negative sentinel lymph node biopsy is
invariably correlated with negative axillary status, except perhaps for T1a-b
breast cancers, with a size of < or =1 cm. Randomized clinical trials should
elucidate the impact of avoiding axillary node dissection on patients with a
negative sentinel lymph node on the long-term clinical outcome of patients.