Infection/Inflammation
Osteomyelitis
See section on "Infection"
Septic Arthritis
Although septic arthritis can occur at any age, it is more common in young children (up to age 2), or adults with underlying joint disease. Monoarticular involvement is the most common pattern (90%). The most commonly involved joint is the hip in children, and the knee in adults. The most common organism is S. aureus. In children, other organisms encountered include: beta-hemolytic strep., gram negative bacteria, and H. influenzae type B (particularly in children less than 12 months old). Clinical findings include fever, pain, swelling, and erythema of the involved joint. In children, the affected hip is flexed, abducted, and laterally rotated (this position permits the largest volume of fluid in the joint). Rapid cartilaginous destruction can ensue and fibrous or bony ankylosis can eventually occur. Other complications include avascular necrosis (which may be related to local septic embolization and vascular compression by effusion), early osteoarthritis (due to cartilaginous destruction), and spread of the infection to the subjacent bone (osteomyelitis). Prompt drainage and antibiotic treatment is essential to prevent cartilage loss and other complications. Etiologies include hematogenous spread, direct inoculation from penetrating injury, or contiguous spread from an adjacent osteomyelitis. This latter etiology is frequently seen in infants under 18 months of age due to the presence of trans-physeal vessels which permit extension of a metaphyseal osteomyelitis to the epiphysis. Spread to the joint then occurs due to a shared blood supply by the epiphysis and the synovium.
The differential for septic arthritis includes transient synovitis which is commonly seen in children less than 10 years old, and characteristically follows a preceding viral URI. A joint effusion is commonly seen and usually resolves within a few days. Varying scintigraphic patterns have been associated with transient synovitis ranging from normal (most common) to 3-phase increased activity.
Early plain film evaluation of septic arthritis of the hip may demonstrate the presence of a joint effusion with joint space widening (greater than 2 mm difference from side to side), superolateral subluxation of the femoral head, or displacement of the capsular fat pads. Demineralization can be seen due to the associated hyperemia, or the presence of a metaphyseal osteomyelitis. Later, there is joint space loss followed by osseous destruction.
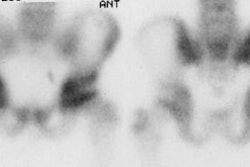
On 3-phase bone scan the inflamed joint demonstrates diffusely increased flow and blood pool activity. Delayed images generally demonstrate increased activity within the bone on either side of the joint. Differentiation from cellulitis may be difficult, but in cellulitis the underlying bone typically demonstrates only a mild increase in tracer activity. Septic arthritis is also suggested if the abnormality on bone scan is clearly synovial in distribution. Occasionally, decreased tracer uptake on delayed images may be seen in the femoral capital epiphysis as a result of vascular compression by the joint effusion. Once the elevated intraarticular pressure is relieved by arthrocentesis, uptake should return to the femoral head [1].
On MRI, up to 60% of cases of uncomplicated septic joint were associated with marrow signal changes that can be mistaken for osteomyelitis.
Synovial Inflammatory Disorders:
Both joint scanning (using Tc-pertechnetate) and blood pool images obtained with Tc-MDP will demonstrate increased tracer activity at sites of synovial inflammation. Gallium and In-111 WBC's will also accumulate at these sites. Differentiation of a septic arthritis from a non-infectious synovial inflammation is not possible by scintigraphy. Aspiration of the joint with culture of the synovial fluid is the best method for diagnosis.
Bone scan is also of limited value in the evaluation of juvenile rheumatoid arthritis. The prominent uptake of tracer within the growth plates often obscures increased periarticular tracer uptake, especially in small joints. In the knee, the lateral view may help to demonstrate increased activity in the patella as it projects free from the growth plate in this view.
Sacroiliitis:
The diagnosis of sacroiliitis is often very subjective. Sacroiliitis, particularly if bilateral and relatively symmetric, can be difficult to detect due to the normal increased activity within the SI joints. Some authors feel that a SI joint to sacrum ratio of greater than 1.35 is abnormal, but others feel that quantitative indices are not reliable in differentiating normal from abnormal activity within the SI joints.
Langerhan's Cell Histiocytosis:
Langerhans' Cell Histiocytosis (formerly referred to as Histiocytosis X) comprises a group of reticuloendothelioses which are not truly neoplasms but which are characterized by a varied and abnormal proliferation of histiocytes. The spectrum of clinical and pathologic entities included in this diverse group of diseases include isolated bone involvement (solitary and multifocal, Eosinophilic Granulomas), the relatively benign disseminated disease ((Hand -Schuller-Christian disease), and the highly malignant form (Letterer-Siwe disease). Musculoskeletal manifestations occur 78% of the time. With skeletal involvement, there is a predilection for marrow involvement with the flat bones of the skull and ileum being the most frequently involved.
On scintigraphy, up to 30 to 40% of skeletal lesions may not be detected, and 10% may appear cold. Nonetheless, bone scan is considered by some to be complimentary to skeletal radiography in this disorder. ROC analysis shows that skeletal scintigraphy has the greatest diagnostic accuracy in the skull, facial bones and mandible (88% sensitivity and 52% specificity). The sensitivity of skeletal scintigraphy for detection of lesions in the pelvis, sacrum, ribs, sternum, scapula, and clavicle is poor [3].
The typical radiographic appearance of Langerhans' Cell Histiocytosis (LCH) is that of a lucent lesion, sometimes well circumscribed, often with a sclerotic border and a beveled edge. Characteristic beveled lesions occur in the skull and the ileum because of differential destruction of the inner and outer table of the skull and the anterior and posterior surfaces of the ileum. Other radiographic appearances of LCH on skeletal surveys include sclerotic lesions, mixed lytic and sclerotic lesions and complicated lesions such as those involving vertebral compression fractures. On skeletal scintigraphy, LCH typically appears as a focus of intense radiotracer uptake or alternatively as a circumscribed rim of increased radiotracer activity surrounding a central region of photopenia.. After local radiotherapy or systemic chemotherapy, the radiotracer distribution is typically more diffuse and often less avid [3].
In a retrospective study of 56 patients treated at the Mayo Clinic during 1965-1994 with a definite lesion on radiographs and biopsy-proven LCH, Howarth et al reported the sensitivity and specificity of the radiographic skeletal survey of 100% and 61%, respectively, compared to 91% and 55% for bone scintigraphy. For solitary lesions, radiographic sensitivity and specificity were 95% and 73%, respectively, compared with 88% and 77% for bone scintigraphy. These authors support the use of the radiographic skeletal survey in the diagnosis and staging of LCH, but suggest that scintigraphy may be useful in monitoring the response of bone lesions to treatment, particularly in the case of solitary bone lesions [3].
Necrotizing (Malignant) External Otitis:
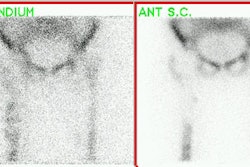
NEO is a fulminant Pseudomonas infection of the external auditory canal complicated by a temporal bone osteomyelitis which affects mainly diabetic patients. Topical treatment is ineffective in these cases. SPECT imaging is essential as it helps to separate bone involvement from adjacent soft tissue activity. Delayed (24 hours) images are also useful due to poor soft tissue clearance typically seen in diabetic patients. Lesion to non-lesion count ratios at 4 and 24 hours utilizing SPECT imaging can help in differentiating NEO from a severe external otitis. Although Ga-67 and In-111 WBC's are more sensitive in the detection of infection, they cannot differentiate between bone and soft tissue involvement. After making the diagnosis of NEO, however, Ga-67 or In-111 WBC's can be used to follow the course of the infection as bone scans will often remain positive for prolonged periods of time despite effective treatment [4].
Recurrent Multifocal Osteomyelitis:
Despite its name, recurrent multifocal osteomyelitis is a rare condition in which the osseous findings mimic that of osteomyelitis, but no pathogens can be isolated from the involved areas. The disorder typically has a benign, self-limited clinical course with periodic exacerbations and remissions. Bone biopsy is mandatory for the diagnosis and demonstrates extensive fibrosis and inflammatory cells, but is culture negative. Patients usually present in late childhood or early adolescence with a single, locally painful, tender and swollen joint- most commonly in the tibia. Complications can include premature physeal fusion and growth disturbances. The disorder has been associated with a rare cutaneous disorder known as palmoplantar pustulosis. Antibiotics have no impact on the course of the disease which usually resolves spontaneously with time. Symptomatic relief can be provided with non-steroidal anti-inflammatory agents.
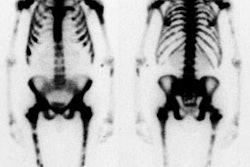
On scintigraphy, multifocal symmetric areas of increased tracer accumulation can be seen in up to two-thirds of cases. [2]
REFERENCES:
(1) J Nucl Med 1998; Connolly LP, et al. Assessing the limping child with skeletal scintigraphy. 39: 1056-1061
(2) J Nucl Med 1998; Mandell GA, et al. Bone scintigraphy in the detection of chronic recurrent multifocal osteomyelitis. 39: 1778-1783
(3) J Nucl Med 1996; Howarth DM, et al. Bone scintigraphy evaluated in diagnosing and staging Langerhans' cell histiocytosis and related disorders. 37(9):1456-60
(4) J Nucl Med 1994; Hardoff R, et al. Semiquantitative skull planar and SPECT bone scintigraphy in diabetic patients: differentiation of necrotizing (malignant) external otitis from severe external otitis. 35: 411-15