
Evolutionary rather than revolutionary changes were the rule at RSNA 2003. Most vendors at the Chicago meeting focused on enhancing existing systems rather than introducing entire new platforms.
One exception was the CT market, where several companies launched 32, 40, and even 64-slice scanners as the next generation of technology beyond the 16-slice systems that represented the state of the art just a year before.
In MRI, gradient-coil channel counts are rising and parallel processing is becoming more common, leading to faster exam times and increased functionality. Three-tesla scanners continue to make inroads into clinical imaging, and could represent the high end of the clinical imaging segment in the years to come.
 |
|
Traffic at dusk on Lake Shore Drive into Chicago.
|
Other technologies continued to evolve. Computer-aided detection (CAD) software is transitioning from software found on a dedicated standalone workstation into an advanced image processing application found on a PACS network. RIS and PACS applications are evolving into a single, integrated entity, which is sure to confer workflow and efficiency benefits to users.
The following is a rundown of some of the clinical highlights from the 2003 meeting.
CT
U.S. researchers sought to determine the prognostic value of CT perfusion imaging in determining the value of thrombolytic therapy in acute stroke patients. By calculating cerebral blood flow and volume in various regions of the brain during acute stroke, it is possible to identify patients for whom thrombolytic therapy should or should not be recommended, they said. A study from Germany reported that the size of the infarct area in a patient with an ischemic stroke would indicate the likelihood of hemorrhage if thrombolytic therapy was introduced.
Meanwhile, in lung imaging, U.S. radiologists found that CT screening to find early lung cancers in high-risk individuals not only discovers the lesions at an early stage of development but also appears to be able to perform the task in a cost-effective manner.
The Early Lung Cancer Action Project (ELCAP) conducted multiple annual CT screenings on 2,968 high-risk subjects, with more than 80% of the diagnosed lung cancers they found classified as stage 1. The CT screens cost $200-$400 each. Cost-effectiveness calculations indicate that a population-based screening program would cost $2,500 for each patient-year of life saved, far below estimates of the threshold cost-effectiveness that, in the United States, is about $50,000 per patient-year of life saved.
In cardiac CT, a committee of radiologists, physicians, and vendors from the U.S. and Europe proposed replacing the Agatston score for coronary calcium measurement with a calcium mass-based standard. The committee believes the new protocols are an improvement on Agatston scoring because it can be used on both electron-beam tomography (EBCT) and multislice CT scanners, and have even been standardized to provide the same measurements regardless of scanner manufacturer. The new standard faces a challenge, however, in that its accuracy has been based mostly on the results of phantom studies.
Screening CT has been a hot topic in the U.S. of late, but a multicenter U.S. group presented a study that might give some women food for thought before they step into the scanner for a screening exam. They found that, depending on the procedure, the radiation dose absorbed by the breast for some CT screening exams was anywhere from two to 19 times that absorbed during a standard four-view mammography exam.
For example, the average radiation dose per breast was 3.7 rads for a coronary calcium scoring scan, and 1.8 rads for whole-body screening. That compares to 0.2 rads per breast for a conventional mammography screening study. Average radiation doses for virtual colonoscopy and lung cancer screening were more in line with mammography -- 0.94 rads during virtual colonoscopy and 0.41 rads during lung cancer screening.
Meanwhile, Korean investigators presented their work aimed at developing optimal exposure protocols for isotropic liver imaging using multidetector-row CT, including slice collimation, reconstruction intervals, and slice thickness.
They found that slice collimation of 0.625 mm with reconstruction interval and slice thickness of 1 mm were the best values for sharpness, but the worst for graininess. In terms of artifacts, the 1.25-mm reconstruction interval was the best value in each group, whereas the 2.5-mm reconstruction interval was the worst, with statistical significance.
 |
|
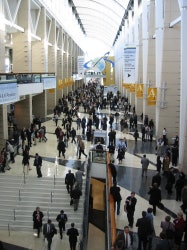
Attendees streaming between the North and South Exhibit Halls on the second day of RSNA 2003.
|
At a reconstruction interval of 0.625 mm, 2.5-mm-collimation images contained significantly fewer artifacts than other collimation settings. In lesion detectability, there were no statistically significant differences; however, 0.625-mm collimation and 5-mm slice thickness showed the worst lesion detectability compared to other collimations and slice thicknesses. They concluded by suggesting that the optimal values for isotropic images of the liver were 1.25 mm slice collimation, 1.25 mm reconstruction interval, and 3-mm slice thickness.
A Canadian group used CT to find a correlation between anorexic women and emphysema-like changes in the lungs. Only 30% of the 18 women in the study who were diagnosed with anorexia nervosa had normal lung inflation, compared with 70% of controls. Anorexic women were also more likely to have poor gas exchange. The researchers plan to follow the study participants for two years to see if restoring their normal nutrition will reverse the lung damage.
Mammography
Many mammography centers have been looking to full-field digital mammography (FFDM) to bring them into the digital age, and a group of U.S. researchers found that FFDM systems also confer benefits by delivering lower radiation dose to patients. At the same time, though, they found that FFDM units from different manufacturers can vary widely in terms of the amount of radiation dose they produce.
FFDM units yielded a mean glandular breast dose per view that was 24% lower than for screen-film mammography (SFM). FFDM systems based on slot-scanning technology had the greatest dose reduction. Flat-panel digital units produced less dose reduction, but were still an improvement over screen-film mammography.
On the other hand, FFDM users had a higher rate of requiring additional exposures beyond the standard four views, with 18.4% of FFDM cases requiring more exposures compared with 13.4% for screen-film. There was also significant variance by manufacturer in the additional-exposure rates.
In other FFDM studies, Norwegian researchers said they found no significant difference in the cancer detection rate between screen-film mammography and FFDM in a screening study of over 3,600 women. Overall, 39 cancers were scored as positive on one or both modalities, with SFM detecting 32 and FFDM finding 28.
The researchers attributed the missed cancers to improper postprocessing of the images rather than observer error. However, new workstation designs, computer-aided detection (CAD), and reader training should boost cancer detection rates on FFDM, they said.
In a second study by the same group, the researchers measured the impact of each mammography modality on reader performance. One reader performed better with SFM, while five did better with FFDM.
German researchers, meanwhile, presented results from the ongoing European SCREEN-TRIAL of soft-copy reading, focusing on whether education can improve radiologists’ performance in soft-copy reading of FFDM exams.
Overall, the results of phase one indicate that asking radiologists to do soft-copy reading without training is less than beneficial. The key to improving soft-copy reading will be more extensive education, the researchers said. In addition, technical issues, such as a potential degradation of microcalcifications on soft-copy images, need to be addressed in order to study observer performance accurately.
Molecular Imaging
Hybrid PET/CT scanning is all the rage in medical imaging, due to its ability to visualize both anatomical and functional changes. In one RSNA paper, German researchers pitted PET/CT against MRI to see which performed better for tumor staging, in particular stage-adapted therapy, which integrates tumor staging (T), lymph node metastasis staging (N), and distant metastasis staging (M).
They found that each modality had strengths and weaknesses. PET/CT performed better in T-staging, with 87% accuracy versus 60% for MRI. For N-staging, PET/CT also excelled, with an accuracy of 93% versus 83% for MRI. The modalities were nearly identical in M-staging, with PET/CT recording accuracy of 92% and MRI 91%.
But the modalities scored differently in different organs. MRI was the most accurate modality for staging liver and bone metastases, while PET/CT scored higher for pulmonary metastases. The authors concluded by stating that they believe PET/CT is ready to be used as a first-line tool for oncologic staging.
The same group also sought an alternative to positive oral contrast agents such as iodine for PET/CT imaging; the positive agents can induce artifacts into the PET emission data if PET attenuation correction is based on the CT scan. They investigated three negative oral contrast agents for dual-modality PET/CT imaging: barium, plain water, and a mannitol/locust bean gum compound made onsite. The researchers found that the mannitol/locust bean gum compound was easy to prepare and showed promise as a negative oral contrast agent, providing good stomach and bowel distension while avoiding potential contrast-induced PET artifacts.
MRI
MRI is becoming an important tool for the assessment of stroke prior to thrombolytic therapy, and U.K. researchers discussed their development of a three-minute protocol that uses an ultrafast MRI technique with an eight-channel array head coil. The shorter scan also produced fewer motion artifacts and yielded additional information regarding arterial anatomy and clot position. The researchers hope to add a perfusion sequence to their protocol, which would add about 90 seconds to the total imaging time.
Austrian researchers reported on initial results from a national screening trial that used MRI to assess breast cancer in women at high risk for the disease. They found that MRI appears to be superior to mammography and ultrasound for screening carriers of the BRCA 1 and 2 genes, and can help in early diagnosis in this patient population. They plan to next study those with a familial history of breast cancer but no documented BRCA mutations.
In a related Italian study, researchers tested breast MR in high-risk women who were either BRCA 1 or 2 carriers or had a strong family history. After scanning 153 women, MRI found 11 of 12 cancers with four false-positives. Of the dozen cancers, 67% were detected only by MRI. The group concluded that women with a strong family history of breast cancer would benefit from annual MR screening, independent of genetic testing
MR spectroscopy proved useful to U.S. researchers, who used the technology to predict the course of disease in patients with multiple sclerosis. They found that by studying N-acetyl aspartate (NAA) levels, researchers may also be able to tell how well medications and investigative therapies are performing in controlling the progressive disease.
According to the results, NAA declined 3.6 times faster in MS patients than in controls over time, indicating that neuronal cell injury precedes brain atrophy. The researchers believe that measuring NAA levels with MRS could aid in the development of MS drugs, particularly to see if the pharmaceuticals are effectively controlling the disease.
RIS/PACS
 |
|
The technical exhibit floor of RSNA 2003.
|
Canadian researchers analyzed the impact of RIS/PACS integration on their hospital system's workflow, productivity, and patient care. At one site in the hospital system, median delays between image production and reading of pulmonary radiographs declined from five days to three days.
At a second site, delays dipped from three to two days with the aid of PACS/RIS, while a third site saw median delay for abdominal CT studies decline from 2.59 days to 2.01 days after RIS/PACS installation. Decreased delays in reading time were seen in both high-volume (chest x-ray) and low-volume (e.g., CT) sectors. The impact of RIS/PACS was more marked in high-volume sectors and at less-efficient sites, they said.
Ultrasound
According to U.S. researchers, Doppler ultrasound examinations conducted early in the first trimester of pregnancy can identify fetal heart anomalies similar to congestive heart failure in adults -- a defect that might be implicated in 40% of early miscarriages. They said that Doppler evidence of fetal defects in heart fluid exchange is 98% accurate at predicting early loss, while the defect's absence predicts that 99% of pregnancies will progress to the fourth month.
On the socioeconomic side, U.S. researchers found that ultrasound use by cardiologists grew three times as fast as by radiologists between 1993 and 2001. Utilization rates among other physicians grew twice as fast as it did among radiologists during the same time period, they said. The researchers said that physician self-referral was probably the cause of the high imaging utilization rates among non-radiologists.
Virtual colonoscopy
Virtual colonoscopy proponents were heartened by the results of a landmark study by U.S. military researchers. They found the CT colon exam to be slightly more sensitive than conventional colonoscopy for the detection of colorectal pathology among average-risk patients.
The group examined more than 1,200 asymptomatic patients with virtual and conventional colonoscopy on the same day, and used 3-D images for initial interpretation rather than reserving it for problem-solving after 2-D review. VC's sensitivity was 91.5% for polyps 6 mm and larger, compared to 88.1% for optical colonoscopy. The use of a stool-tagging oral contrast agent may have also improved the results.
A separate U.S. group put another feather in virtual colonoscopy's cap by demonstrating a high predictive value for the presence of colorectal masses after failed colonoscopy. Some 3%-10% of conventional colonoscopies fail to reach the cecum, which leaves the virtual exam as the brightest hope for finding significant colorectal abnormalities. They performed virtual colonoscopy on 625 patients following failed colonoscopy -- endoluminal findings 6 mm or larger were seen in 99 patients (13.4%), and of these, they found 13 masses larger than 20 mm in 13 patients, 12 of which were positive and one that was negative at follow-up colonoscopy.
By AuntMinnie.com staff writers
Copyright © 2004 AuntMinnie.com



















