Norbert Pelc, ScD, professor of radiology at Stanford University School of Medicine in Stanford, CA, described some of the technology developments that have emerged over the past couple of decades. He pointed out the steady shift in clinical MRI from 1.5 tesla to 3 tesla, with the reducing cost and increasing reliability of 3-tesla magnets leading to an increase in the number of higher-field-strength systems.
Other clinically adopted trends include an increase in bore diameter and decrease in magnet length, features that increase patient comfort. "The wider- and shorter-bore systems that have become popular are largely achieved by more effective magnet design and squeezing the coil stack-up," he explained. "We've also seen a significant trend in massively parallel receiver coils, driven by parallel imaging and the desire to reduce scan times."
In research settings, the penetration of higher field strengths, although still small, is ongoing, Pelc noted. Systems incorporating 7-tesla magnets, for example, offer increased signal-to-noise ratio, enabling faster scans or higher-resolution imaging. Higher field strengths also offer greater spectral separation for MR spectroscopy. However, such machines are large, expensive, and complex. "Will these penetrate into the clinic?" he asked. "We don't know yet, but further cost reduction could be achieved if more were produced."
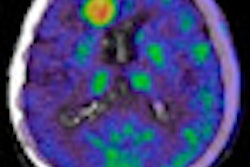
As for areas under active investigation, Pelc cited the development of parallel transmit systems, and the emergence of an increasing number of hybrid instruments that combine MR with other diagnostic or therapeutic modalities. These include systems for MR-guided thermal therapy and radiation therapy, as well as dual-modality imaging devices such as MR/PET and x-ray/MR hybrids.
Finally, Pelc highlighted work on hyperpolarization, in which increasing the nuclear spin polarization far beyond thermal equilibrium conditions results in up to a 105 to 106 increase in MR signal. "MR technology development is alive and well," he affirmed.
Advanced applications
It's not just the technology that's developing. MRI applications continue to evolve alongside. "We've had 30 years of steady progress in MRI, and the range of information provided by MR continues to increase," said John Gore, PhD, professor of radiology and radiological sciences and director of the Vanderbilt University Institute of Imaging Science in Nashville, TN. "If you look at the trends over the past 10 years, we now use imaging to study function rather than just anatomy."
Gore told AAPM delegates how much of the research in this field is focused on the development of imaging biomarkers, defined as characteristics that can be measured and evaluated as indicators of a biological process. Such processes include, for example, blood flow, angiogenesis, perfusion and diffusion of cellular water, as well as response to drugs or other treatments.
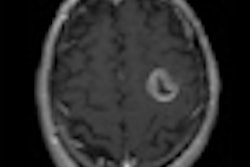
Within oncology, MRI is currently used both to detect and stage tumors. Emerging applications include characterization of an individual tumor to assess whether it is likely to respond to a particular treatment, and monitoring of therapeutic response. "We have a number of evolving cancer markers, particularly for assessing treatment response," said Gore.
Tissue properties such as perfusion and hypoxia, for example, can be examined using dynamic contrast-enhanced (DCE) MRI. Analyzing the time course of the MR signal at each pixel reveals changes in tissue vascularity properties with time, or in response to treatments, enabling DCE to function as a quantitative biomarker of angiogenesis.
Another cancer indicator, proliferation, can be assessed with diffusion MRI, which tracks the movement of water molecules within tissue. Monitoring the apparent diffusion coefficient (ADC) before and after treatment reveals changes in cellularity (high cellularity restricts diffusion and results in a lower ADC), which can be used as an indicator of treatment response.
MR spectroscopy, meanwhile, provides a biomarker for metabolism, revealing the relative abundances of different metabolites. While MR spectroscopy signal levels are intrinsically too low to use for imaging, hyperpolarization techniques -- such as injection of a hyperpolarized carbon-13-labeled agent -- could enable practical use. Gore noted that the first trials of this technique in human subjects are taking place this year.
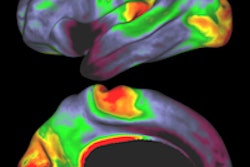
MRI is also used within neuroimaging. Current applications include cerebral blood flow measurement and the use of diffusion-tensor imaging (DTI, a form of diffusion MRI) to quantify the degree of myelination in the brain.
Functional MRI, based on BOLD (blood oxygen level dependent) signals, can detect changes in the brain while the subject performs tasks. It could also be applied to measure changes in brain activation patterns in response to administered drugs. Here, the use of higher field strengths should enable single-subject studies. Such "pharmacological MRI" has reached the stage where the effects of drugs are being studied in patients. "This could have a major impact in neurology and psychology," said Gore.
"Measurements of novel imaging biomarkers are likely to be of broad use in selecting treatments, assessing response, and assessing individual effects of drugs. Future applications will involve the developing and use of quantitative imaging biomarkers," Gore concluded. "I think that the ideas on how to use MRI will continue to keep pace with the technical advances."
By Tami Freeman
Medicalphysicsweb editor
August 9, 2010
Related Reading
AAPM: MRI, lasers used for novel cancer treatment, July 22, 2010
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community Web site covering fundamental research and emerging technologies in medical imaging and radiation therapy.