AI may have a role in finding contralateral disease in women with a personal history of breast cancer, according to findings published April 8 in Radiology.
A team led by Su Min Ha, MD, PhD, from Seoul National University Hospital in South Korea reported that AI by itself achieved a higher performance than radiologists with no AI help when it came to detecting contralateral breast cancer in women treated with unilateral mastectomy.
“It may be feasible to apply a commercially available [AI] algorithm to the standalone detection of contralateral breast cancers in patients treated with unilateral mastectomy, with AI achieving a higher cancer detection and sensitivity than that of radiologist interpretation alone,” the Ha team wrote.
AI continues to show promise in improving screening mammography interpretation. However, the researchers noted a lack of data on interpreting surveillance mammograms in women with a personal history of breast cancer.
Surveillance mammography in this patient population has lower sensitivity and higher interval cancer rates than conventional screening mammography. These interval cancers have poorer prognosis and may include larger tumor size, negative hormone receptor status, and positive lymph node status.
Ha and colleagues compared the performance of a standalone AI system (Lunit Insight, version 1.1.7.1; Lunit) with that of two breast radiologists with no AI assistance for second breast cancer surveillance in women treated with unilateral mastectomy. The radiologists had 10 and 17 years of experience, respectively.
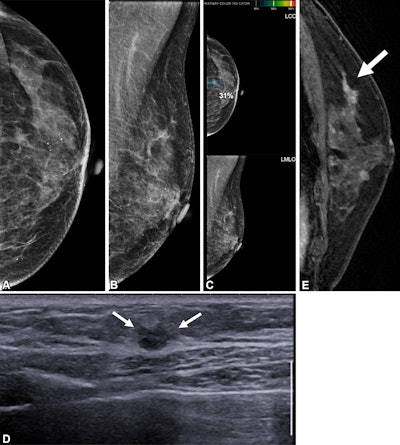 Images depict a 65-year-old patient with contralateral second breast cancer 6.3 years after right mastectomy. (A) Left craniocaudal and (B) mediolateral oblique mammograms assessed as benign. (C) The AI algorithm outlined a lesion with a score of 31 on the craniocaudal view. (D) A supplemental axial ultrasound scan, which was obtained on the same day as the mammogram, shows an irregular hypoechoic mass (arrows) in the left upper central breast. (E) Preoperative sagittal contrast-enhanced T1-weighted MRI scan shows the corresponding enhancing mass (arrow) in the left upper center. The mass was proven to be ductal carcinoma in situ.RSNA
Images depict a 65-year-old patient with contralateral second breast cancer 6.3 years after right mastectomy. (A) Left craniocaudal and (B) mediolateral oblique mammograms assessed as benign. (C) The AI algorithm outlined a lesion with a score of 31 on the craniocaudal view. (D) A supplemental axial ultrasound scan, which was obtained on the same day as the mammogram, shows an irregular hypoechoic mass (arrows) in the left upper central breast. (E) Preoperative sagittal contrast-enhanced T1-weighted MRI scan shows the corresponding enhancing mass (arrow) in the left upper center. The mass was proven to be ductal carcinoma in situ.RSNA
Final analysis included data collected from 4,184 asymptomatic women with an average age of 52 years. Of these, 111 (2.7%) had contralateral second breast cancer. The women were diagnosed between 2001 and 2018 and underwent post-mastectomy surveillance mammography between 2011 and 2023.
| Performance of AI, radiologists with no AI assistance in detecting contralateral breast cancer in women with a personal history | |||
|---|---|---|---|
| Measure | Radiologists | Standalone AI | p-value |
| Cancer detection rate (per 1,000 exams) | 14.6 | 17.4 | 0.01 |
| Sensitivity | 55.0% | 65.8% | 0.01 |
| Specificity | 98.1% | 91.5% | < 0.001 |
The AI system also detected 16 of 50 (32%) cancers missed by radiologists. However, both AI and the radiologists missed 34 of 111 (30.6%) breast cancers. The study authors highlighted that this finding “underscores the need for further studies to support the translation of this promising technology into routine clinical practice.”
They added that one ideal approach to using AI in this area is to use it as an interactive tool during radiologist interpretation
“This approach could help prevent overlooking cancer findings or interpretation errors while simultaneously reducing false-positive findings caused by either radiologists or AI,” the authors wrote. “Further prospective studies on the interpretation of surveillance mammography with AI aid are warranted.”
In an accompanying editorial, Liane Philpotts, MD, from Yale University in New Haven, CT, wrote that these results provide useful information into how AI functions in a specific clinical scenario. This can aid other researchers as they continue to develop their AI models, though Philpotts added that standalone AI is “probably still a distance off.”
“There may be no single ‘AI fits all,'” she wrote. “Fine-tuning AI algorithms remains a challenging problem for the very challenging art of mammography interpretation.”
The full study can be found here.