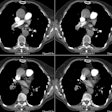
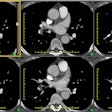
A new view of pulmonary edema and acute respiratory distress syndrome.
Ketai LH, Godwin JD
The old division of lung edema into two categories--cardiogenic (hydrostatic) and noncardiogenic (increased permeability)--is no longer adequate. For instance, it fails to distinguish between the capillary leak caused by acute respiratory distress syndrome from that caused by interleukin-2 treatment. Further, it fails to account for the capillary leak ('stress-failure') that may accompany edema. A modern view of edema must recognize the natural barriers to the formation and spread of edema. These barriers are the capillary endothelium and the alveolar epithelium. Varying degrees of damage to them can account for the varying radiographic and clinical manifestations of lung edema. Thus, interleukin-2 administration causes increased endothelial permeability without causing alveolar epithelial damage. The result is lung edema that is largely confined to the interstitium, causing little hypoxia and clearing rapidly. However, acute respiratory distress syndrome, which is characterized by extensive alveolar damage, causes air-space consolidation, severe hypoxia, and slow resolution. Thus, a reasonable classification of lung edema requires at least four categories: 1) hydrostatic edema; 2) acute respiratory distress syndrome (permeability edema caused by diffuse alveolar damage); 3) permeability edema without alveolar damage; and (4) mixed hydrostatic and permeability edema. The authors emphasize the importance of the barriers provided by the capillary endothelium and the alveolar epithelium in determining the clinical and radiographic manifestations of edema. In general, when the alveolar epithelium is intact, the radiographic manifestations are those of interstitial (not air-space) edema; this radiographic pattern predicts a mild clinical course and prompt resolution.